Analgesia (Paediatric Guidelines)

- Use the oral route whenever possible.
- Verbal consent should be obtained from the child and/or parent if the rectal route is to be used. Also if the child has had bowel surgery, check with the surgeon that the rectal route may be used.
- Prescriptions for regular opioids should be reviewed by anaesthetic/pain team / medical staff daily.
- When changing from one route of administration to another, use “step-over” doses (equipotent) until you can assess the effect. Later you can change to “step-down” drugs (less potent) when appropriate.
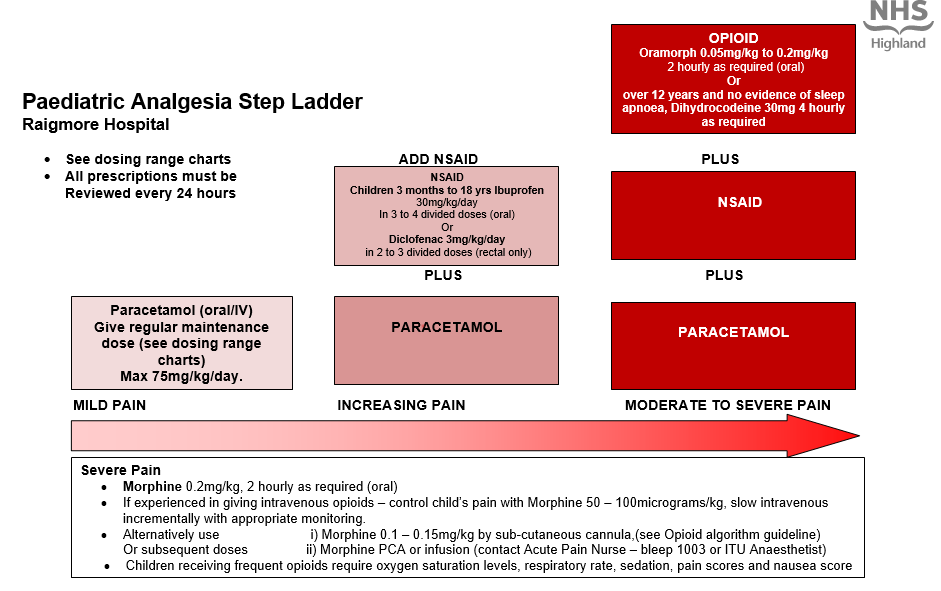
- Give Paracetamol and NSAID’s regularly as prescribed and opioids as required. A multi-modal approach improves pain relief and reduces the child’s opioid requirement.
- Do not prescribe compound analgesics for children. eg. Co-codamol.
- All prescriptions must be reviewed every 24 hours
Paracetamol dose in children - oral route
- Paracetamol can be administered by the oral routeREGULARLYfor the relief of mild to moderate pain and as an adjunct to stronger analgesics in severe pain.
- If the patient has not received any paracetamol in the preceding 24 hours, a loading dose of 20mg/kg (prescribed on the ‘ONCE ONLY’ section of the drug kardex) may be used if necessary, followed by the usual dose.NB this is included in the patient’s total daily dose.
- Do not exceed 1g in a single dose or 4g in 24 hours.
- All Children should be dosed by weight rather than age. If the weight is unknown then follow the dosing by age in the BNF for Children.
| Age | Dose | Interval | MAXIMUM DAILY DOSE |
Pre-term neonate 28-32 weeks corrected gestational age | 10mg/kg | 8 hourly up to three times daily | 30mg/kg/day |
Neonate over 32 weeks corrected gestational age | 15mg/kg | 6 hourly up to four times daily | 60mg/kg/day |
1 month to 18 years | 15mg/kg up to a max of 1g | 4 hourly up to four times daily | 75mg/kg/day |
Paracetamol dose in children - rectal route
- When the oral and the IV routes are not available, Paracetamol can be administered by the rectal route but dosing can be complex as bioavailability is very variable.
- If the patient has not received any paracetamol in the preceding 24 hours, a loading dose of 30mg/kg may be given followed by the usual dose
- Child 1 month to 18 years 15- 20mg/kg per dose
- Suppositories should not be halved.Doses are adjusted according to the suppository strength available.
- Maximum of 4 doses may be given in 24 hours.
- The maximum daily dose is 75mg/kg/day, up to max of 4g daily (for 5 to 12 years as per BNFc).
| Age | Dose | Interval | MAXIMUM DAILY DOSE |
1 to 3 months | 60mg | Every 4 hours | 75mg/kg/day |
3 to 12 months | 60 to 120mg | Every 4 hours | 4 doses in 24 hours (or 75mg/kg/day) |
1 to 5 years | 120 to 240mg | Every 4 hours | 4 doses in 24 hours (or 75mg/kg/day) |
| 5 to 12 years | 240mg to 500mg | Every 4 hours | 4 doses in 24 hours (or 75mg/kg/day. Maximum 4g daily) |
12 to 18 years | 12 to 18 years | Every 4 hours | 4 doses in 24 hours |
Paracetamol dose in children - IV route
- When the oral route of administration is unavailable, IV preparations of paracetamol should be considered.
- IV paracetamol is no more potent or effective than oral paracetamol but dosing is reduced in certain circumstances due to a greater potential for toxicity.
- All IV doses should be administered as a slow IV infusion over aminimum of 15 minutesto avoid hypotension.
- Do not exceed 1g as a single dose or 4g in a 24 hour period.
- Consideration should be made to decreasing the maximal dosing further in the presence of hepatic impairment, malnutrition, dehydration and muscle disorders.
| Patient | Dose | Interval | MAXIMUM DAILY DOSE |
Pre-term Neonate over 32 weeks corrected gestational age | 7.5 mg/kg | 8 hourly | 22.5mg/kg/day |
Term Neonate | 10 mg/kg | 4 hourly, up to three times daily | 30mg/kg/day |
Child under 10kg | 10 mg/kg | 4 hourly, up to three times daily | 30mg/kg/day |
Child 10 to 50kg | 15 mg/kg | 4 hourly, up to four times daily | 60mg/kg/day |
Child over 50kg | 1g | 4 hourly, up to four times daily | 4g/day |
NSAIDs may have adverse effects so care should be taken when determining if NSAIDs are suitable for patients and when prescribing/ reviewing therapy. Please check through the list below before prescribing NSAIDs.
Non-steroidal anti-inflammatory Dosing in children
IBUPROFENcan be administered by theoral routeevery 6 to 8 hours.
The dose is 5 mg/kg up to 30 mg/kg/day.
Cautions – see list on NSAID flow chart
| Age |
Standard Dose |
Standard Interval
|
Maximum Dose |
|
1 to 3 months |
5mg/kg |
6 to 8 hourly |
up to four times daily |
|
3 months to 18 years |
5mg/kg up to 400mg |
6 to 8 hourly, up to three times daily |
7.5mg/kg as a single dose up to 30mg/kg/day |
PREPARATIONS AVAILABLE:
Suspension: 100mg/5ml
Tablets: 200mg and 400mg
DICLOFENAC
If the oral route is not available then DICLOFENAC can be administered by the rectal route.
| AGE | DOSE | INTERVAL | COMMENT |
|
6 months to 18 years |
0.3 to 1mg/kg up to 50 mg |
8 hourly | The dose must be adjusted according to the suppository strength available |
PREPARATIONS AVAILABLE:
Suppositories: 12.5mg, 25mg, 50mg
Oral Opioid Doses
Age | Dose | Interval |
6 months - 17 years | Oramorph | Up to 2 hourly |
Over 12 years | Dihydrocodeine | Up to 4 hourly |
Oral opioids have the same side effects as parenteral opioids and the following need to be carried out:
Routine post-operative observations: pulse, oxygen saturation levels, respiratory rate, pain score, sedation score and nausea score should be recorded on the observation chart.
- Assess effects half an hour after each administration of opioid
Oxygen saturation levels less than 94% on air (with no other known cause)
- Administer oxygen by facemask, commence with 4 litres per minute and titrate until sats >95% and ensure a clear airway.
- Stay with the child and monitor respiratory rate, sedation and oxygen saturation levels continuously.
- Contact the On call/duty anaesthetist for further advice.
- Assess for other causes of hypoxia/sedation.
- Reduce subsequent dose of opioid by half and assess if the child's pain can be managed with regular paracetamol and/or NSAIDS (oral/rectal).
Respiratory depression
Oral opioids have the same side effects as parenteral opioids and the following need to be carried out:
| Age | Breaths per minute |
| Less than 6 months | below 20 breaths per minute |
| 6 months to 2 years | below 16 breaths per minute |
| 2 years to 7 years | below 14 breaths per minute |
| 8 years and over | below 10 breaths per minute |
- Ensure a clear airway and administer oxygen 4 litres per minute via face mask and titrate until sats >95%.
- Stay with the child and monitor the respiratory rate, sedation and oxygen saturation levels continuously.
- Contact the paediatrician and On Call/Duty anaesthetist for further advice.
- Assess for other causes.
- Reduce subsequent doses of opioids by half and assess if the child’s pain can be managed with paracetamol and /or NSAIDS.
Severe respiratory depression
| Age | Breaths per minute |
| Less than 6 months | below 18 breaths per minute |
| 6 months to 2 years | below 14 breaths per minute |
| 2 years to 7 years | below 12 breaths per minute |
| 8 years and over | below 8 breaths per minute |
- Ensure a clear airway and administer oxygen face mask, commence with 4 litres per minute and titrate until sats >95%.
- Contact the paediatrician and On Call/Duty anaesthetist to review urgently.
- Administer Naloxone (10 micrograms/kg IV in increments. e.g for a 30kg child the maximum dose of Naloxone is 300mcg. Give ¼ of the dose and repeat after 1 minute intervals if there is an inadequate response until the maximum dose of Naloxone has been given. A Naloxone infusion may be required.
- If the response to Naloxone is inadequate then consider other causes.
- The child must be nursed in the high dependency area until opioids are no longer required. Continuous pulse oximetry must be used.
- Reduce subsequent doses of opioids by half and assess if the child’s pain can be managed with paracetamol and /or NSAIDS.
Side effect management
Constipation
- Laxatives should be prescribed for any child receiving regular opioids.
- Ensure a high fibre diet and adequate fluid intake
- Assess for other causes
Nausea and Vomiting
- If a child complains of nausea or is vomiting please give the prescribed anti-emetic
- See paediatric post operative nausea and vomiting (PONV) guidelines
- Children receiving regular opioids may require regular prophylactic anti-emetics
- If problem continues despite treatment as per guidelines consider iv fluid therapy to maintain hydration
Itching
- Assess cause – it may not be the opioid- rash with dressings etc
- Prescribe antihistamine as required – Chlorphenamine Doses:
Child 2 – 6 years 1mg, every 4-6 hours. Max 6 mg daily.
6 – 12 years 2mg every 4-6 hours. Max 12mg daily.
12 – 18 years 4mg every 4-6 hours. Max 24mg daily
Use Opioids with caution in the following groups of children as they may need a reduced dose and longer dosing interval
- Children with moderate to severe renal impairment.
- Children with moderate to severe liver impairment.
- Children with sleep apnoea, upper airway abnormalities or those at risk of upper airway obstruction.
- Children with severe neurological disorders
Oxycodone oral solution
Oxycodone oral solution (1mg/ml) can be used as an alternative strong opioid when morphine is contraindicated. This is not a stock medication and must be ordered in advance through pharmacy. The dosing regimes in the BNFc are for moderate to severe oncological pain and a 30-50% dose reduction may be more appropriate for treatment of moderate post-operative pain.
- Morphine 0.2mg/kg, 2 hourly as required (oral)
- If experienced in giving intravenous opioids – control child’s pain with Morphine 50 – 100mcg/kg, slow intravenous incrementally with appropriate monitoring.
- Alternatively use i) Morphine 0.1 – 0.15mg/kg by sub-cutaneous cannula, (see Opioid algorithm guideline)
- Or subsequent doses ii) Morphine PCA or infusion (contact Acute Pain Nurse – bleep 1003 or On call/Duty Anaesthetist)
- Children receiving frequent opioids require oxygen saturation levels, respiratory rate, sedation, pain scores and nausea score
