Cardiovascular disease risk is an important factor to consider for those with T2DM. Treatment selection for hyperglycaemia should consider whether a person has:
- established ASCVD (ischaemic heart disease, stroke); or
- cardiovascular risk factors of:
- QRISK2 more than 10% in adults aged 40 and over (or other validated tool); or
- a clinically assessed elevated lifetime risk of cardiovascular disease (defined as the presence of 1 or more of the below cardiovascular risk factors in someone under 40)
- hypertension;
- dyslipidaemia;
- smoking;
- obesity; or
- family history (in a first-degree relative) of premature cardiovascular disease.44
See Algorithm for management of Type 2 diabetes mellitus.
Any modifiable risk factors for ASCVD (hypertension, hyperlipidaemia, smoking, obesity) should be addressed. For useful links to lifestyle information see the list 'Lifestyle support resources' in Lifestyle interventions and remission.
Prescribing choices
- Metformin remains first line.
- SGLT-2i should be prescribed for individuals with established ASCVD43, heart failure or chronic kidney disease. Individuals at high risk who have not yet developed these complications may also benefit.
- A shared decision-making approach is recommended, considering:
- beneficial effects e.g. weight loss, extent of glucose-lowering efficacy;
- adverse effects e.g. in relation to the degree of hyperglycaemia, or the risk of hypoglycaemia; DKA
- preferences e.g. route of administration, oral verses injectable, frequency of administration, daily or weekly
SGLT-2i contra-indications/cautions:
- people 75 years and older are at increased risk of volume depletion
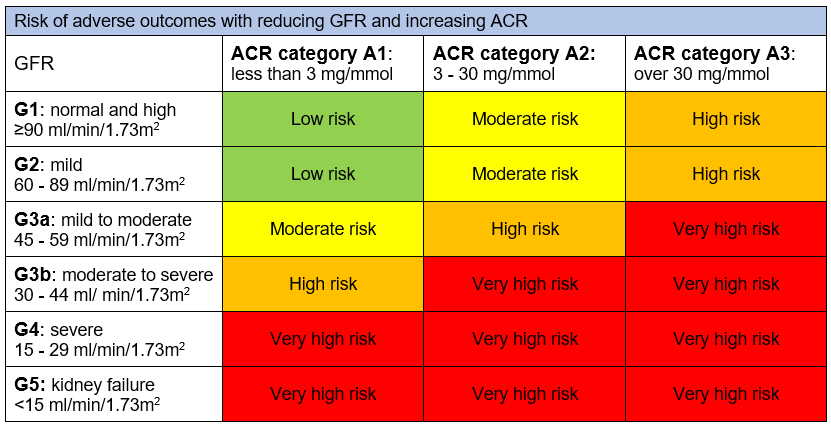
- not recommended for initiation when eGFR is <15 ml/min/1.73m2
- have less glucose-lowering efficacy with eGFR <45 ml/min/1.73m2
- should be avoided in those with:
- factors predisposing to DKA/eDKA
- pancreatic insufficiency
- drug or alcohol misuse disorder
- a low/ultra-low carbohydrate or keto diet
- excessive alcohol consumption
- frequent bacterial urinary tract infections or genitourinary yeast infections
- low bone density or high risk for falls/fractures
- current foot ulceration.
Increased incidence of euglycaemic diabetic ketoacidosis
With increasing use of SGLT-2i, there has been an increased incidence of eDKA in addition to DKA. Therefore the MHRA45 has issued the following advice:
- use SGLT-2i with caution in those with risk factors for DKA, (including a low beta cell reserve, conditions leading to restricted food intake or severe dehydration, sudden reduction in insulin, increased insulin requirements due to acute illness, surgery or alcohol misuse), and discuss these risk factors with individuals
- test for raised ketones in individuals with signs and symptoms of DKA, even if glucose levels are near-normal
- discontinue treatment if DKA is suspected or diagnosed
- do not restart treatment with any SGLT-2i in those who experienced DKA during use, unless another cause for DKA was identified and resolved
- during and after surgery or during acute serious illness:
- interrupt sodium-glucose co-transporter 2 (SGLT2) inhibitor treatment in patients who are hospitalised for major surgical procedures or acute serious medical illnesses
- monitor ketones during this period – measurement of blood ketone levels is preferred to urine
- restart treatment with the SGLT2 inhibitor once ketone values are normal and the patient’s condition has stabilised.
Furthermore emerging advice46,47 regarding the period of treatment interruption is:
- For three days prior to planned surgery (four days if prescribed ertugliflozin), (or immediately if unplanned surgery) and for a further three days after surgery
- During acute illness, e.g. diarrhoea, vomiting (see sick day guidance).
Individuals considering an SGLT-2i should be advised about the risks of eDKA associated with a low/ultra-low carbohydrate or keto diet.
See Case study 3.
Due to the different licenses for SGLT-2i (and GLP-1RAs), prescribers should familiarise themselves with the indications and contra-indications as well as interactions listed in the BNF and/or the Electronic Medicines Compendium before initiating therapies.
Where there is no difference between drugs within a class, the most cost-effective drug should be chosen, and NHS boards should consider their formulary choices.
The recent NICE2 guideline Type 2 Diabetes in adults: management supports the introduction of SGLT-2i as first-line therapy with metformin, if the individual has chronic heart failure or established atherosclerotic cardiovascular disease. These drugs should be started sequentially, with metformin first, then once tolerability is established, the SGLT-2i can be started.
Cardiovascular disease and risk should be reviewed regularly, and may require a change/addition in therapy. See the summary algorithm for the management of type II diabetes mellitus.