Cataract (Guidelines)

Patient presentation
Cataract is a clouding of the lens of the eye which causes a reduction in vision. The most common cause is ageing but cataracts may also be caused by an inflammatory eye disease or trauma and often develop earlier in patients with diabetes. The visual impairment may start as glare / burning in bright light and can, if untreated, lead to blindness.
Age related macular degeneration is another common cause of visual impairment in later life and it is the main differential diagnosis. Cataract and AMD may coexist and therefore a judgement has to be made as to whether the cataract is paying a significant role to warrant surgery.
Further information from RNIB on eye conditions can be accessed here
Sight Action
38 Ardconnel Street
Inverness
IV2 3EX
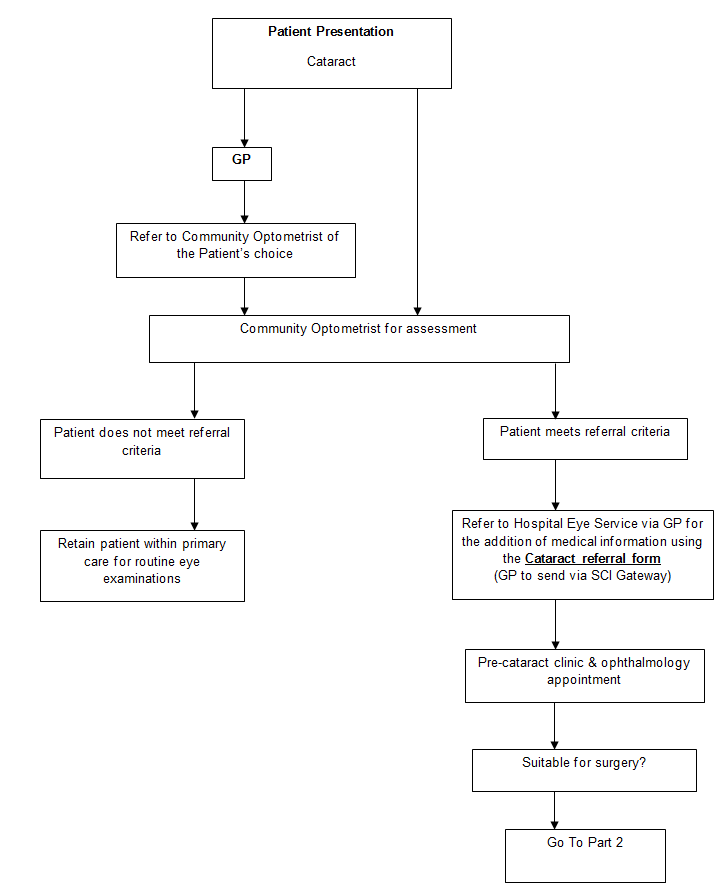
All patients complaining of a gradual decrease in vision should be referred to a community optometrist.
The Department of Health in the National Eye Care Plan supports referral by Community Optometrists as the preferred referral method
- History & symptoms
- Refraction & visual acuity & pupil reflexes
- Slit lamp examination
- Tonometry & visual fields
- Dilated fundus examination
- Detect/exclude any co-morbidity
- Discuss risks and benefits of surgery
- Issue information leaflet to patient
- Agree desire for surgery with patient
- Refer on standardised referral form via local GP (for general health & medication details to be added)
If the diagnosis is a cataract the patient should be informed that the only treatment is surgery and that surgery can be done at any stage and it does not harm the eye to wait, nor does waiting strain the other eye.
The risks of surgery should be discussed with the patient: The risk of total loss of vision due to a post operative infection or other catastrophic event is 1 in 500. The risk of other less serious complications is around 1 in 100.
The patient may be helped to arrive at a decision by considering whether the visual disability present causes difficulty in life style, driving especially.
The intraocular pressure and dilated fundus examination should be assessed.
- Cataract sufficiently dense to produce subjective impairment of vision manifesting as:
- dim vision
- glare in sunlight or driving at night
- difficulty reading or performing specific tasks
- difficulty with kerbs or steps.
- The patient wishes to be considered for surgery
- Visual acuity reduced & causing impairment in lifestyle.
- If blepharitis is present, this should be treated before referral.
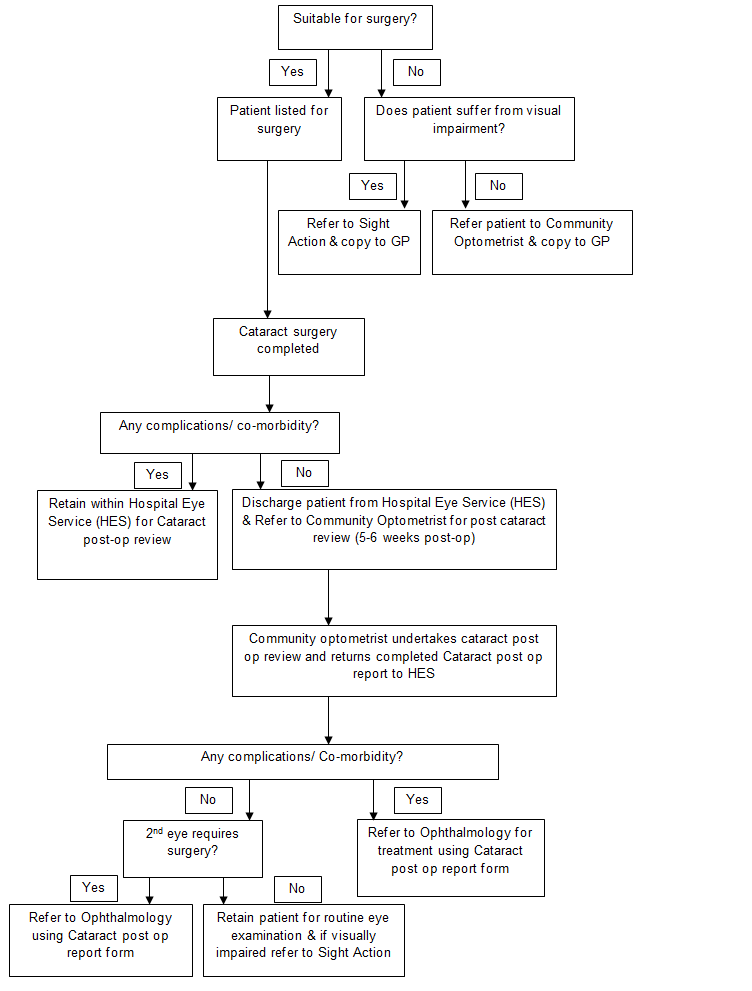
Pre-cataract assessment (Nurse-led clinic): Risk factors, medical and social history, vision, visual acuity, biometry, blood pressure, body temperature, IOP, focimetry of current spectacles, patient education, transport arrangements for the day of surgery and assessment of the patients ability to instil eye drops following surgery are discussed.
Ophthalmology/Optometry: Slit lamp examination, dilated fundus examination, patient consent form completed
Optometric examination:
- History & symptoms
- Refraction & visual acuity & pupil reflexes
- Slit lamp examination
- Tonometry & visual fields
- Dilated fundus examination
- If complications: Refer to Ophthalmology
- If second eye required cataract extraction (Phaco & IOL)
- Discuss risks and benefits of surgery
- Issue information leaflet to patient
- Agree desire for surgery with patient
(Refer to Optometrists Cataract Post-Op Review Guidelines)
Urgent referral to HES (phone eye clinic)
- Infection (including suspected endophthalmitis)
- Retinal detachment
- Increased IOP >30mmHg
- Wound leakage
- Suture complications (unlikely as sutures rarely needed)
- Iris prolapse/incarceration of vitreous in the wound.
- Moderate-Severe anterior uveitis (inflammatory cells >2+)
Routine referral to HES (standard post-op report form)
- IOL not in place
- Posterior Capsular opacification (PCO). PCO is the commonest complication of cataract surgery. It is caused by the proliferation of lens epithelial cells left behind following cataract surgery. The cells migrate behind the intraocular lens implant (IOL) to obscure the visual axis and reduce the patient’s visual function similar to that experienced with the original cataract. If PCO occurs vision may be restored by laser capsulotomy. As patients are discharged soon after cataract surgery it is essential that they are warned of the potential problem of PCO and advised to seek attention if they feel their vision deteriorates. Regular optometric review will ensure that PCO is detected and further referral to HES may be organised as necessary.
- Corneal oedema
- Increased IOP(<30mmHg)…possible steroid responder.
- Cystoid Macular Oedema (CMO) if no improvement after co-management with GP
- Unsatisfactory refractive error
Co-managed with GP/Optom
- Slight-Moderate anterior uveitis (Inflammatory cells 1+) 4-6 weeks post-op. Community optometrist to write to GP to request prescription for Maxidex qid for 2-3 weeks. Community Optometrist will review after 2-3 weeks and if no improvement after this time will refer to Hospital Eye Service.
- Cystoid Macular Oedema (CMO) 4-6 weeks post-op. Community optometrist to write to GP to request prescription for topical steroid (Maxidex) qid, Ketorolac trometamol 0.5% (G. Acular) qid for 4 weeks and Ibuprofen 400mg 3 times per day for 4 weeks (if no contraindications). Community Optometrist will review after 2-3 weeks and if no improvement after this time will refer to Hospital Eye Service'.
- Corneal toxicity reaction to eye drops (withdraw eye drops)
- Corneal abrasion'
