|
History
|
Examination
|
|
Poor urine flow (particularly for boys)*
|
High risk/serious illness suspected
|
|
Previous UTI
|
Age under 3months*
|
|
Antenatally diagnosed renal anomaly
|
Enlarged Bladder*
|
|
Family history of vesicoureteric reflux (VUR) or renal disease
|
Abdominal Mass*
|
|
Constipation
|
Poor Growth
|
|
Dysfunctional Voiding
|
Evidence of Spinal Lesion*
|
|
Recurrent fever of uncertain origin
|
High Blood Pressure* (Box 1 below)
|
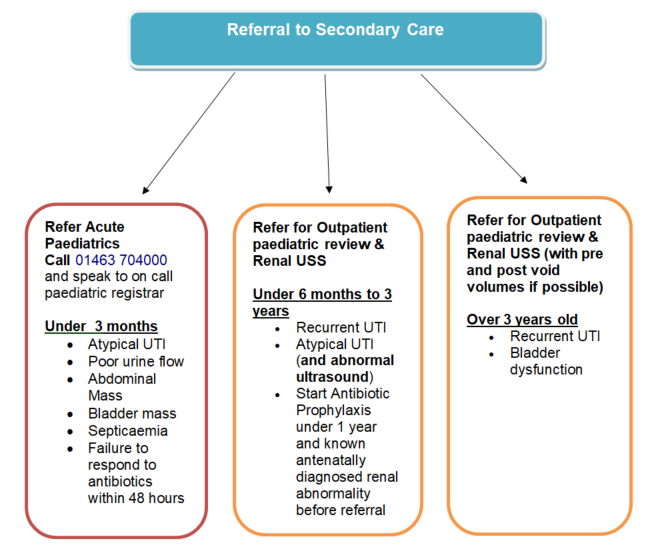
* Urgent referral to paediatrics, on-call registrar, via 01463 704000 (Raigmore Hospital switchboard)
BOX 1: Average systolic blood pressures by age (rough guide)
|
Age (years)
|
Average Systolic Blood Pressure
|
|
1 to 2
|
80 to 95
|
|
2 to 5
|
80 to 100
|
|
5 to 12
|
90 to 110
|
|
Over 12
|
100 to 120
|
Reference: The Hands-on Guide to Practical Paediatrics, First Edition. Rebecca Hewitson and Caroline Fertleman. © 2014 John Wiley & Sons, Ltd. and APLS 6e
Definitions of UTI (BOX 2)
|
Upper UTI /Pyelonephritis
|
Lower UTI/cystitis
|
Recurrent UTI
|
Atypical UTI
|
- Fever: 38°C or over
- Lethargy
- General Malaise
- Vomiting
- Loin Pain
|
- Non specific abdominal Pain
- Frequency Urgency
- Dysuria
- Enuresis
- Frank Haematuria
|
TWO Upper UTI within 12 months
OR
ONE Upper UTI + ONE lower UTI within 12 months
OR
THREE or more lower UTI within 12 months
|
*Seriously ill
*Poor urine flow
*Abdominal or bladder mass
*Raised creatinine
*Septicaemia (fluid bolus + IV antibiotics)
*Failure to respond to appropriate antibiotics in 48 hrs
*Infection with non-E.coli organisms.
|
- Uncomplicated UTI (a terminology used sometimes): UTI in patients who have a normal, unobstructed genitourinary tract, no history of recent instrumentation and symptoms are confined to the lower urinary tract.
Urine collection - core principles.
- A clean catch urine sample is the recommended method for urine collection in infants and young children (non-toilet trained) and a mid-stream urine in an older child. Cleaning genitalia with water, prior to urine collection, is required.
- In infants, there is some evidence for the “Quick-Wee method” (fig. 1) for clean catch urine collection. It involves gentle, suprapubic, cutaneous stimulation using a gauze soaked in cold fluid for 5 minutes, which might significantly hasten bladder voiding in infants 1 to 12 months of age. Needless to say, before doing this, it is essential to be ready with a sterile bowl to catch the voided urine!
- Fig. 1 Quick-Wee method:

- If a clean catch urine sample is unobtainable, non-invasive methods such as urine collection pads may be used, strictly following the manufacturer’s instructions. DO NOT use urine bags, cotton wool or gauze due to high risk of contamination.
- Urine samples should preferably be taken prior to starting antibiotics.
- If symptoms and signs highly suggestive of UTI and/or dipstick positive for leucocytes and/or nitrites, the urine should be sent for microscopy and culture.
Note: Nitrites might be falsely negative in young infants and children who are not toilet trained as urine does not sit long in the bladder to form nitrites.
- In a severely unwell infant/ child, treatment should not be delayed if the urine sample is unobtainable.
- Urine samples for microscopy and culture should be collected in a red-top urine container (contains boric acid) and care taken to prevent overfilling (can destroy bacteria and cause false negative results). Ensure lid is replaced tightly (can leak and will not be processed).
Box 3: Urine Dipstick for diagnosis: (L = leucocyte esterase, N = Nitrites)
|
Result
|
Urine for microscopy and culture?
|
Start Antibiotic?
|
|
L+ N+
|
Yes
|
Yes
|
|
L- N+
|
Yes
|
Yes
|
|
L+ N-
|
Yes
|
3 years and under - Yes (if symptoms specific for UTI)
Over 3 years - await urine culture
|
|
L- N-
|
No
|
No (unless strong suspicion of UTI/risk factors*)
|
*See Box 5
Note: Leukocyte esterase positive on dipstick may be indicative of an infection outside the urinary tract in a febrile child which may need to be managed differently.
Box 4: Interpretation or Urine Microscopy results in conjunction with culture
| Microscopy results |
Pyuria positive |
Pyuria negative |
| Bacteriuria positive |
The infant or child should be regarded as having UTI |
The infant or child should be regarded as having UTI |
| Bacteriuria negative |
Antibiotic treatment should be started if clinically UTI |
The infant or child should be regarded as not having UTI |
- Significant Pyuria > 10 x 106 /L of urine; Bacteriuria is often referred to the bacteria on microscopy or on culture.
Urine Culture criteria for diagnosis:
- Urine culture is easier to interpret when urine sample is taken before antibiotics.
- Confirmed UTI = Significant growth = pure growth >105Colony forming units (CFU)/ml. Any growth on a urine from suprapubic aspirate is significant.
- Do NOT routinely repeat urine culture after finishing antibiotics, if the child has clinically improved.
- Do NOT [test urine (!) and] treat Asymptomatic Bacteriuria
Box 5. Urine samples should be sent for culture:
- Suspicion of acute pyelonephritis/upper UTI
- High to intermediate risk of serious illness/ Infants under 3 months
- In infants and children under 3 years: positive leukocyte esterase only (but specific signs of UTI present).
- High suspicion of UTI and/or underlying renal abnormality.**
- In infants and children with recurrent UTI.
- In infants and children with an infection that does not respond to treatment within 24 to 48 hours, if no sample has already been sent
- When clinical symptoms and dipstick tests do not correlate.
$$: Non-Ecoli pathogens may not induce significant pyuria. If high clinical suspicion of UTI, urine for culture must be sent and chased for definitive diagnosis.
Blood Tests:Full blood count, Urea, Electrolytes, Creatinine, Bicarbonate, Liver function tests, Calcium, Magnesium, Phosphate, CRP.
C-reactive protein alone should not be used to differentiate acute pyelonephritis/upper urinary tract infection from cystitis/lower urinary tract infection in infants and children.