Acute symptoms usually last 24-36 hours and can be treated with short term anti-emetics. On-going sensation of imbalance may last 2 to 3 months. Gradual mobilization should be encouraged and medication avoided if possible as may slow rehabilitation.
Treatment : Symptomatic relief and mobilize as able.
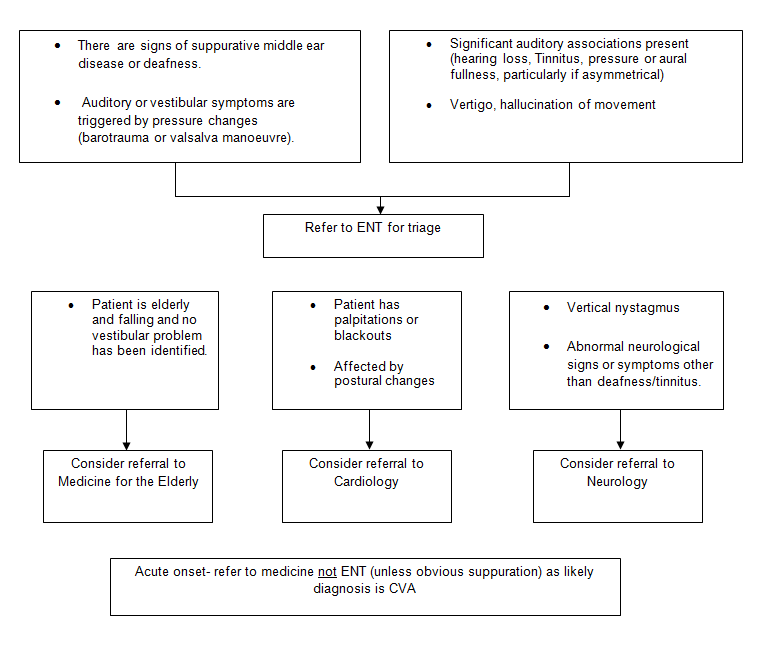
If no subjective improvement after this time, consider referral to ENT for triage