The UK national guidance document ‘Surgery and Opioids’ (see resources) is a detailed document on opioid stewardship and underpins this guidance on opioid prescription after surgery.
Surgical patients are nearly four times more likely to get post-discharge opioids than their non-surgical counterparts. Between 3% and 10% of opioid naive patients become chronic users after surgery.
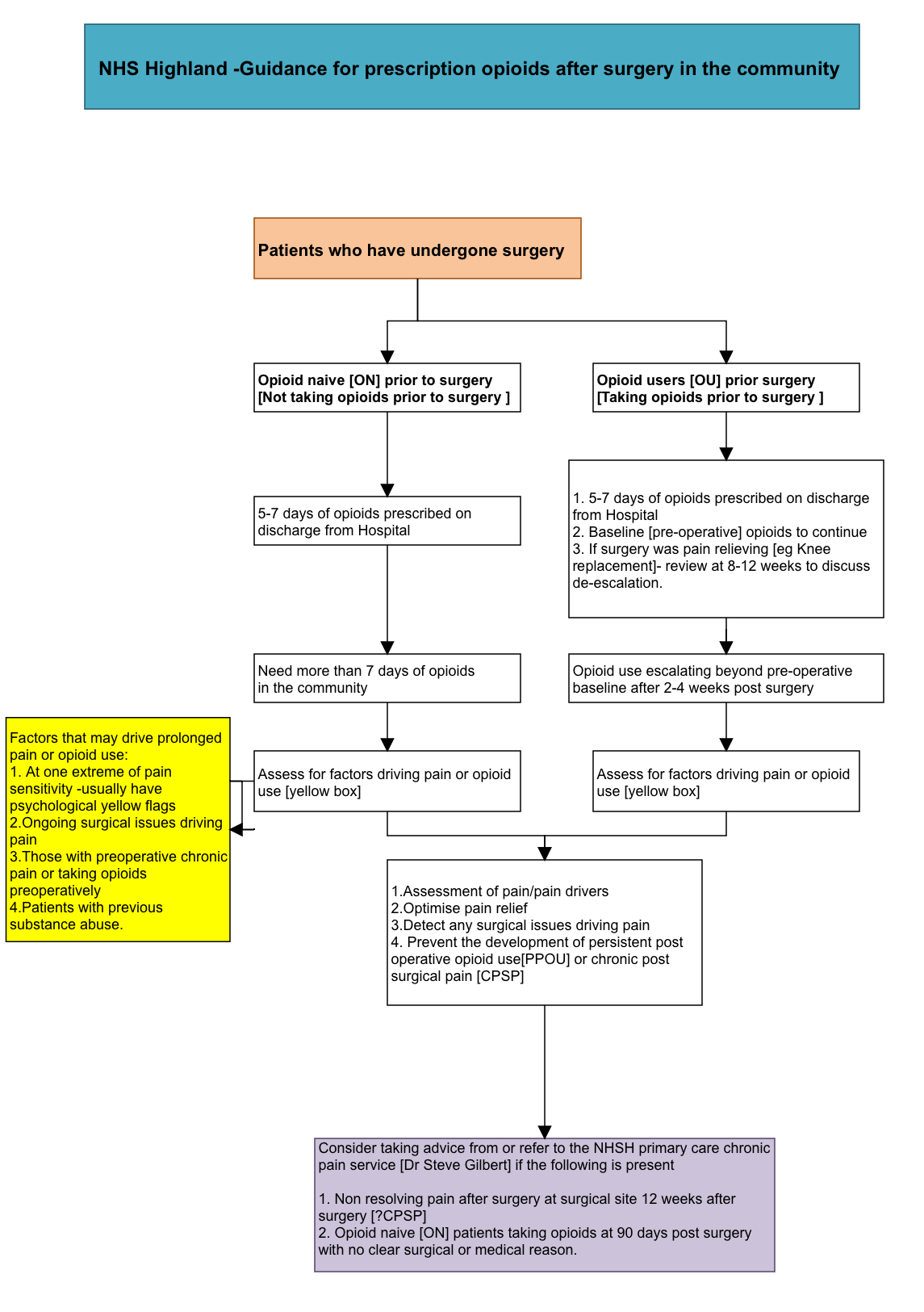
It is important to differentiate two groups of patients with respect to post-surgical opioid prescribing. The first group of patients are the ‘opioid naïve’ (ON) group ie these patients were not taking opioids prior to their surgery. The second group are the ‘opioid users’ (OU) ie those who were taking opioids prior to surgery.
The majority of surgical patients are expected to have a pain score less than 4/10 on day 7 post-surgery. The majority of patients need about 5 to 7 days of opioid supply post-operatively in the community.
The UK national guidance states:
- Usually 5 days and no more than 7 days of opioids (including tramadol) should be prescribed.
- The hospital discharge letter must explicitly state the recommended opioid (including tramadol), the dose and the duration.
Patients discharged from hospital should receive the leaflet ‘Understanding and managing pain after surgery’ (see resources).
Post discharge from hospital
If ON patients need opioids for more than 7 days after surgery, a review is required by a skilled healthcare professional. For this minority of surgical patients, an assessment of the factors that might be driving post-operative pain needs to be assessed and an optimal pain relief regimen prescribed. This might mean prescribing opioids beyond 7 days if necessary but keeping it under constant review and reducing opioids as appropriate.
It follows that the patients needing more than 7 days opioid after surgery (minority) have one of the following issues :
- These patients are at the extreme end of the bell curve for pain resolution after surgery and usually have a yellow flag (psychosocial) issue such as high anxiety, depression or catastrophising pre-operatively or post-operatively.
- Ongoing surgical issues such as infection / surgical abdomen, etc, that need to be assessed clinically.
- Patients with pre-operative chronic pain.
- Patients taking pre-operative opioids (OU).
- Patients with substance abuse
- Early suggestion of development of chronic post surgical pain or persistent post-operative opioid use
For those taking opioids prior to surgery (OU), it is important that their opioid dosages are continued throughout the peri-operative period and supplemented by around 30% to 40% top-up of analgesics during this period. These patients are likely to continue to need their long-term opioid medications beyond the post-operative healing period.
There is a strong case to de-escalate or taper opioids in individuals who have had successful surgeries to relieve pain (eg knee / hip replacement) and no longer need opioid support for their pain. Weaning of opioid medication should be gradual and patients can be reassured that, while there might be some short term withdrawal symptoms, there is good evidence that pain will be no worse. Community based de-escalation has been trialed by the i-wotch trial. For information on opioid weaning, see Faculty of Pain Medicine: Tapering and Stopping (see resources).
In conclusion
For the majority of patients, a 5 to 7-day supply of opioids at discharge from hospital after surgery is optimal. For those who need more than 7 days opioid supply after surgery, a review is necessary to optimise pain relief, detect surgical issues and prevent the development of persistent post operative opioid use (PPOU) or chronic post-surgical pain (CPSP).