Preterm, chronic lung disease, congenital heart disease and airway anomalies.
<5kg ideal, 5-8kg challenging but achievable. No specific upper age limit.

This is a guide / aide memoire for staff preparing for spinal anaesthesia in neonates & infants in theatre at RHC Glasgow.
Please note other departments use different equipment & set-up for lumbar puncture in a similar patient group.
Anaesthetists / Anaesthetic assistants at RHC Glasgow.
Further information please contact: jocelyn.erskine@ggc.scot.nhs.uk or graham.bell@ggc.scot.nhs.uk or the Duty anaesthetist 84842
(after discussing the appropriateness of the technique with the surgeon)
Failure rate when you’re starting is about 1-in-10 to 1-in-30 when you’re good!
All the usual complications. Aseptic meningitis has been reported. Most major complications remain unreported (but possible).
Early apnoea rate greatly reduced compared to GA, late apnoeas are less common and seem to be due to patient (not anaesthetic) factors & there is no difference in incidence compared with GA.
Early evidence of limited developmental consequences related to total anaesthesia exposure in early life, these concerns persist on a google search but we should not use them to promote spinal anaesthesia use in patients.
Spinal anaesthesia does, however, result in favourable haemodynamics compared to GA.

2. Anaesthetic equipment


SUPINE: Assistant stabilises baby from axilla to pelvic brim.


LATERAL: Assistant stabilises the head, other hand under the flexed knees and ‘curls’ the baby. Beware the risk of airway obstruction.

Ensure the drape extends to include the sacral hiatus but no further- aim to keep any unexpected fluids on the ‘dirty’ side.

SPINAL ANAESTHESIA

Top tips:
2 clicks & you’re in.
It’s deeper than you expect & almost never <10mm
Staying in the midline is everything
If you don’t get CSF back when you expect it then withdraw, don’t advance, & withdraw 1mm at a time
Bloody taps often clear to bloodstained CSF
Onset of the block in premmies is near instant but can take up to 10 minutes in a 3 month old
Once spinal sited proceed with caudal. This is optional but does appear to increase the density and duration of the block.
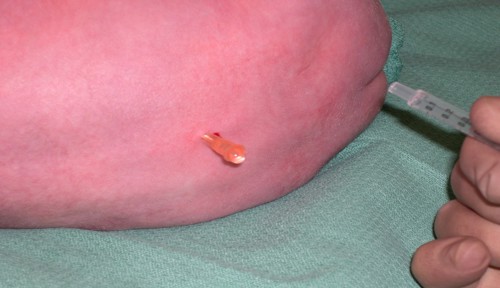
CAUDAL ANAESTHESIA
THEN


Non-restrictive arm suspension
KNIFE TO SKIN
ENVIRONMENT


Being prepared is everything
Issues that occur:
Many of these patients may be returning to NICU for ongoing care/transfer back to base hospital.
However, there may be patients outwith the NICU setting who are eligible for same day discharge. The decision to discharge should be at the discretion of the anaesthetist but factors to consider are:
We are aware of the impending implementation of NR Fit equipment. We do not yet have the equipment available in RHC but updated photos will be obtained and uploaded as soon as we do.