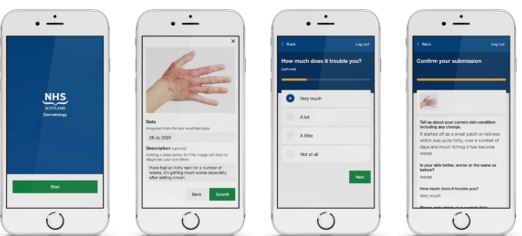
The service was initially developed to be used in return patients initially. However, with the Covid-19 Pandemic the system was then used in new patients with suspected skin cancer, as well as other urgent referrals deemed suitable by the clinician.
Hundreds of patients have now been assessed in this way – 75% new and 25% return. A third of the patients using the service were over the age of 60 and 80% of the images were felt to be of diagnostic quality.
Nearly a third of patients were able to be reassured and discharged from further review. Less than half the patients required further face to face assessment. Others were booked directly for a biopsy or other treatment – allowing faster diagnosis of skin cancers.
Digital consultations have been timed and on average were three minutes quicker than face to face consultations.
Patient feedback was positive and has allowed for refining the suitability of this approach for certain types of case. Many patients would have needed to take time off work for their appointments and this was avoided.
Thousands of miles of travel were also saved. During the first 3 months the team calculated that about 4,000 miles of travel equating 719 kg of CO2 emissions were avoided.
A digital approach doesn’t necessarily suit everyone though and while it may be quicker and more convenient for some, others for whatever reason may not be able to use this system or prefer face to face review. But digital technology can enable this too by improving the efficiency of clinics thereby making face to face review easier. In the DDA system further digital review was required for a proportion (around 40% of those with inflammatory conditions and 7% of those with cancers) and traditional face to face review was still required for almost half.
Dr Donna Torley, who along with her colleague Dr Grant Wylie, leads the NHS GGC development of the service, said “This is just part of our toolkit, it’s not necessarily suitable for all, but for some it’s just as good as face to face, and for some it’s better as it’s more convenient. It enhances our cur clinics as we now offer a mixture of virtual and face to face appointments, tailored to the individual.”
Grant added ‘This pilot platform has streamlined triage for our most urgent and suspected cancer patients allowing everyone the input they need. It has also allowed more personal direct virtual engagement for our well known Return patients. Good photos have also been found to be better than video.”
Other advantages of this approach are that colleagues who are shielding or self-isolating but still able to work can use the system and continue to provide a valuable service.
In fact, during the first year of the pandemic, the dermatology service saw over 260 patients virtually, allowing a reduction in face to face appointments and appropriate safe triaging of other patients proving that a carefully considered collaboration incorporating a digital solution can both personalise care and improve the service we provide: Realistic Medicine in action.