Maternal cardiac arrest

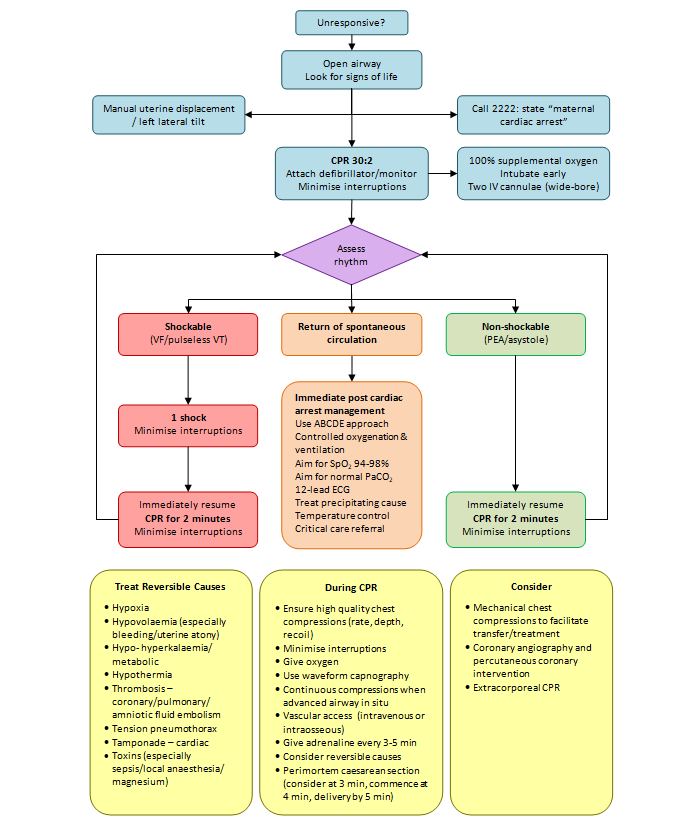
Resuscitation council guidance for Modification for Advanced Life Support in the pregnant patient
- Call for expert help early (including an obstetrician and neonatologist).
- Start basic life support according to standard guidelines.
- Use the standard hand position for chest compressions on the lower half of the sternum if feasible.
- If over 20 weeks pregnant or the uterus is palpable above the level of the umbilicus:
- Manually displace the uterus to the left to remove aortocaval compression.
- If feasible, add left lateral tilt – the chest should remain on supported on a firm surface (e.g. in the operating room). The optimal angle of tilt is unknown. Aim for a tilt between 15 and 30 degrees. Even a small amount of tilt may be better than no tilt. The angle of tilt used needs to enable high-quality chest compressions and if needed allow surgical delivery of the fetus.
- Prepare early for emergency hysterotomy.
- If over 20 weeks pregnant or the uterus is palpable above the level of the umbilicus and immediate (within 4 minutes) resuscitation is unsuccessful, deliver the fetus by emergency hysterotomy aiming for delivery within 5 minutes of collapse.
- Place defibrillator pads in the standard position as far as possible and use standard shock energies.
- Consider early tracheal intubation by a skilled operator.
- Identify and treat reversible causes (e.g. haemorrhage). Focused ultrasound by a skilled operator can be used to identify reversible causes and may also be used to assess if a fetal heart rate is present.
- Consider extracorporeal CPR (ECPR) as a rescue therapy if ALS measures are failing
(https://www.resus.org.uk/library/2021-resuscitation-guidelines/special-circumstances-guidelines)