Asymptomatic Abnormal ALT, GGT or ALP result
Suggested thresholds for investigation when elevated at least 2 occasions > 4 weeks apart.
- ALT > 70
- ALT 50-70 with an abnormal GGT/ALP (if isolated ALT 50-70 check Hep B&C serology only)
- GGT > 100
- ALP > 200 with an abnormal GGT
- (if ALP raised in isolation investigate for bone disease)
(NE: if ALT/ALP/GGT persistently abnormal but below thresholds for investigation consider repeat LFT’s in 1 year. If still abnormal use clinical judgement and consider patient assessment / liver screen even if remains below thresholds).

Patient Assessment
- History
- Examination
- Liver screen liver ultrasound
- Medication review
- If alcohol suspected, advise abstinence

Refer to GI if any of the referral criteria* are met

If the Referral Criteria have not been met then:
- The abnormal LFT’s are likely to be due to either NAFLD or alcohol and there is nothing to indicate advanced fibrosis/cirrhosis.
- These patients can continue to be safely managed in primary care with appropriate advice e.g. diet, exercise, alcohol abstinence.
- A small number will go on to develop cirrhosis if they do not make the appropriate lifestyle changes.
- At present we are unable to identify which people are most likely to progress but FIB 4 score < 1.45 (or <2 if NAFLD and Age > 65) = Fibrosis excluded.
- Consider yearly check of LFT’s and AST:ALT ratio with reinforcement of lifestyle advice.
History
- Alcohol intake
- Drugs (prescribed, OTC, herbal remedies)
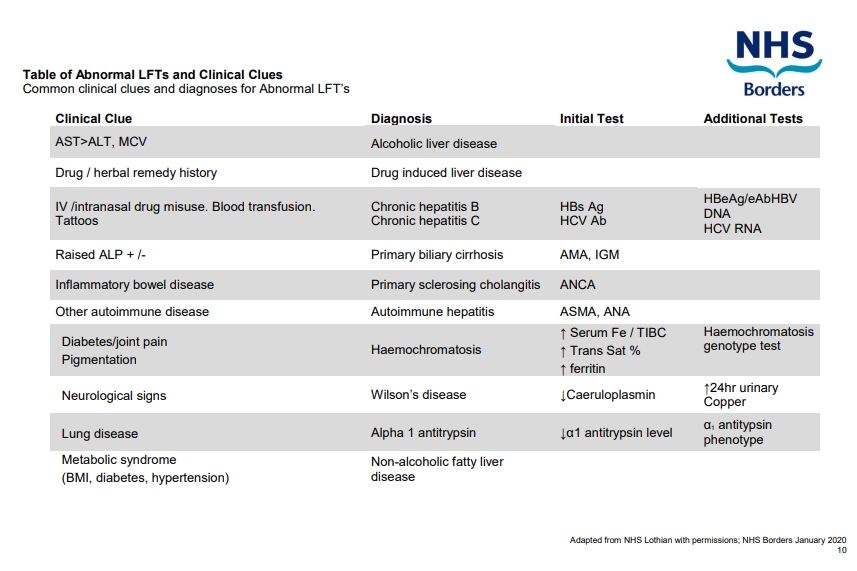
- Hepatitis risk factors (IVDA, sexual history, travel, ethnicity)
- Metabolic syndrome clues (T2DM, obesity, hypertension, hyperlipidaemia)
- Autoimmune disease clues (T1DM, thyroid disease, RA)
- Family history
Examination
- BMI
- Spider naevi, Palmar erythema
- Palpable liver or spleen
Liver Screen
- Abdominal Ultrasound
- FBC
- LRT’s
- AST:ALT ratio
- Albumin
- Immunoglobulin
- Caerulopasmin (if < 55 years)
- α 1 Anti Trypsin
- Glucose
- Cholesterol
- Ferritin (check Transferrin sats if ferritin raised)
- Prothrombin Time (PT)
- Hepatitis serology – HBsAg and anti-HCV Ab
- Immunology – Anti-smooth muscle Ab, anti-nuclear Ab, anti-mitochondrial Ab
Medication Review
Review medications and consider discounting and causative drugs. If in doubt, discuss with GI/Liver.
* GI Referral Criteria
Refer to GI if any of the following apply:
- Diagnostics tests suggest any cause other than alcohol
or NAFLD - Evidence of impaired liver function:

 Bilirubin (not due to Gilbert’s syndrome)
Bilirubin (not due to Gilbert’s syndrome) PT
PT Albumin
Albumin- Evidence of advanced fibrosis/cirrhosis
- AST:ALT ratio > 1.0
- Platelets < 150
- Splenomefaly
- Nodular Liver
- ALT persistently > 200
- Diagnosis or management still uncertain.
FIB 4 score
FIB 4 score is a mathematical method of identifying low risk for fibrosis patients and those with high risk for fibrosis.
- Low fibrosis scores may be appropriate candidates for medical management and may not require liver biopsy if FIB-4 scores continue to stay low.
- Severe fibrosis/cirrhosis scores may need liver biopsy for confirmation of cirrhosis unless there are other clinical or imaging signs of progression to end-stage liver disease.
Hyaluronic acid is a biochemical fibrotic marker available via Lothian.
Where patients have mildly abnormal LFTs, not fulfilling referral guidelines and where the abnormal LFTs are felt to be due to NAFLD or alcohol then a reassuring FIB 4 score and/or hyaluronic acid should guide Primary Care follow up with lifestyle advice and perhaps repeat testing in 2-3 years if appropriate.
One page PDF version of summary


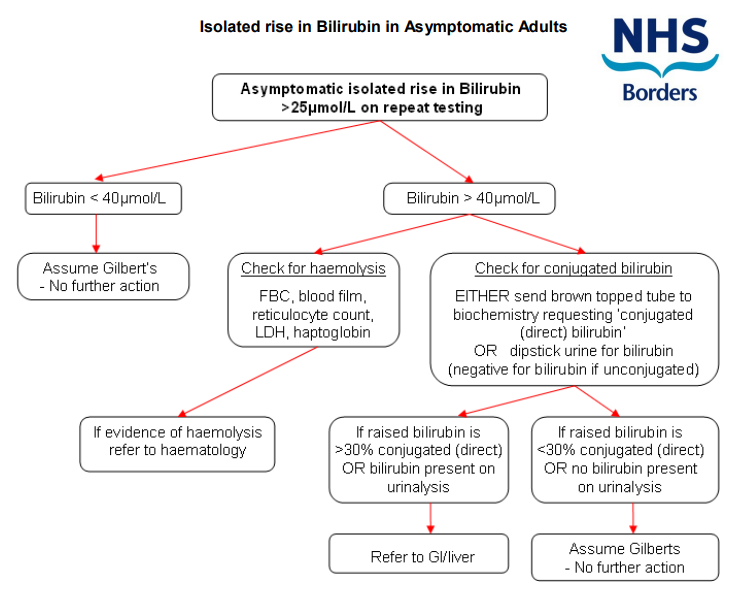
 Bilirubin (not due to Gilbert’s syndrome)
Bilirubin (not due to Gilbert’s syndrome)