To improve the service, start by understanding your baseline. In other words, assess what you currently offer or do around Waiting Well and identify any gaps.
Self-assessment questionnaire
- Use this questionnaire to record your assessment of the current baseline level of support for Waiting Well in your service.
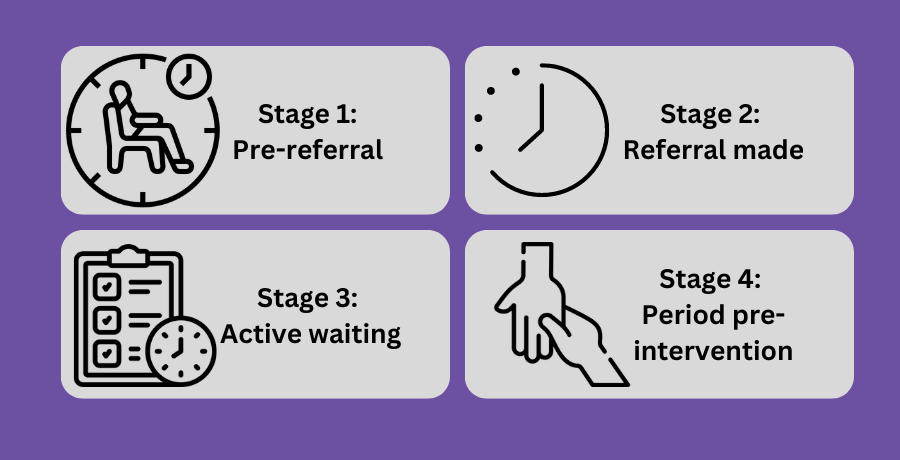
- The questionnaire includes links to useful resources at each stage of the Waiting Well pathway. It also highlights principles and recommendations for action where there are gaps in your service at any stage in the pathway.
- At the end of the questionnaire you will be prompted to enter your email address to receive a record of your self-assessment.