- GGC uses the Scottish Maternity Early Warning Score (SPSP 2018) and current NICE guidance. The parameters and escalation pathways are included in appendices 1 and 2.
- MEWS is the early warning score to be used during the perinatal period. Please see Table 1 below for required documentation in each area.
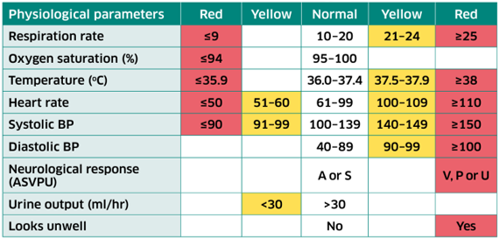
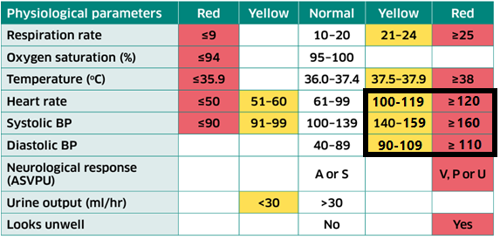
- The physiological observations required for a Maternal Early Warning Score consist of
- respiratory rate,
- oxygen saturation,
- temperature,
- heart rate,
- blood pressure,
- urine output
- neuro response
- looks well or unwell.
Neuro response is scored as
-
- A (Awake);
- S (sleep);
- V (Responds to voice);
- P (Responds to painful stimuli);
- U (Unresponsive- no eye, voice or motor response).
- All observations are required to calculate a MEWS. These are highlighted with a yellow star
 in the observations form on Badgernet. In community settings, where equipment is unavailable, oxygen saturations may be omitted.
in the observations form on Badgernet. In community settings, where equipment is unavailable, oxygen saturations may be omitted.
- A MEWS should be recorded for
- All women attending Maternity Triage
- All women admitted to one of GGC’s maternity units
- All women receiving postnatal community care
- MEWS should be the early warning score used in the Emergency Department and in any acute hospital setting where a pregnant or postnatal women is an inpatient.
- All observations should be recorded in Badgernet. Paper MEWs should only be used in HDU where required. Refer to table below for information on documenting observations in each area.
- Observations entered into labour assessment, MEWs or postnatal observations on Badger will generate a score. It is the responsibility of the person carrying out the observations to ensure the scoring is accurate.
- The visual representation (digital MEWS chart) of the observations should always be viewed in conjunction with entering observations. It can be viewed from the ‘Charts’ section on Badgernet.
- Observations score as Normal, Yellow or Red. Observations outwith Normal are always actionable.
- The frequency of observations should be consistent with the clinical situation and the individual history of the woman (see detail below). The frequency of observations must be considered and modified according to changes in the clinical condition.
- Always consider the possibility of sepsis for women with observations that deviates from normal parameters. If identified, manage as per Maternal Sepsis guideline.
- Reviews and accompanying management plans must be appropriately documented on Badgernet.
- Health Care Assistants, Maternity Care Assistants, and students completing vital signs assessments must report immediately any observations in the yellow or red zone to the midwife responsible for that woman.
- It is the responsibility of the midwifery staff to follow the escalation flow chart. (Appendix 2). When paging medical staff, if there is no response within 5-10 minutes, contact the next level above, until at Consultant level, if necessary.
- It is the responsibility of the medical team to follow the escalation plan, review within the appropriate timeframe and inform senior medical staff if appropriate.
- If a woman does not consent to observations, or becomes resistant to observations, document and escalate. Remember metabolic (e.g. hypoglycaemia) or other serious pathologies (e.g. head injury) may cause atypical behaviours. Consider new confusion as a possible sign of deterioration.
- Use the SBAR format to escalate warning signs of deterioration, yellow or red observations to the multi-disciplinary team.
In summary, comprehensive and accurate documentation of observations will allow timely identification of early warning signs of deterioration. This should prompt the timely and appropriate escalation of concerns to the MDT for management and treatment.
Table 1
|
Antenatal Admissions
|
- All antenatal admissions should have one full set of observations completed and documented on the MEWS chart at their initial review.
- This will be followed by routine observations documented on the MEWS chart as per individual management plan.
- All antenatal observations should be documented under ‘MEOWS/MEWS’ in observation type on Badgernet (appendix 4).
|
|
Triage attendance
|
- All women should have a set of observations recorded and a MEWS calculated on admission to Triage.
- Use of Assessment Unit/Smart Assessment Unit will provide a MEWS. Subsequent observations should be entered as ‘MEOWS/ MEWS’ observations (appendix 4).
- The frequency of observations and MEWS should then be informed by that baseline MEWS and professional clinical judgement according to the clinical situation.
|
|
Intrapartum
|
- All observations during the intrapartum period should be recorded on the partogram using ‘Labour Assessment’. This will pull through to the MEWS digital chart on Badgernet.
- The frequency of observations will be determined by the clinical situation. At a minimum these observations would be an hourly pulse, and 4-hourly temperature, blood pressure and respiratory rate during the first stage of labour. Many women will require more frequent observations. Ensure all fluid output and input is measured and documented during the intrapartum period.
- Observations outwith intrapartum parameters require urgent escalation and action. Note parameters are slightly different during intrapartum period for MEWS and Sepsis triggers. Refer to intrapartum table in appendix 1 for MEWS and sepsis guideline for further information.
|
|
HDU care
|
- Paper MEWS charts can be considered for use in addition to Badgernet documentation for women admitted to HDU.
- If more than one MEWS chart is required then they should be numbered sequentially and filed in the case notes on transfer to the postnatal ward.
- All paper MEWS should be scanned and uploaded to Badgernet.
|
|
Postnatal care
|
- A full set of maternal observations and documentation of MEWS should be completed within 1 hour of 3rd stage completion and repeated prior to transfer to the postnatal ward (or before leaving a woman’s home after a homebirth). Additional/more frequent observations and MEWS may be required if clinically indicated.
- All post-operative women, and women requiring more frequent monitoring than a daily postnatal assessment, should have observations documented as ‘MEOWS/MEWS’ for observation type (appendix 4).
- All uncomplicated vaginal births and women requiring daily observations should have observations documented as ‘Postnatal’ in observation type on Badgernet. Clinicians should be aware that the postnatal assessment on Badger does not include neuro-response, or urine volume in its MEWS calculation. Therefore, if any MEWS are triggered or there are any clinical concerns, observations should return to documentation as ‘MEOWS/MEWS’ to ensure all triggers are completed (appendix 4).
- Refer to postnatal guideline for frequency of observations during the postnatal period. Remember additional/more frequent observations and MEWS may be required if clinically indicated, for example if a woman reports feeling unwell at any postnatal visit.
- Appendix 3 contains guidance for escalation of MEWS outwith normal parameters in a community setting.
|