Refer to Lipid clinic via SCI Gateway...DGRI...Clinical Biochemistry for the following groups:
- Patients with suspected familial hypercholesterolaemia:
- If total cholesterol >7.5 mmol/L and there is a history of cardiovascular disease (CVD) in a first-degree relative aged ≤60 years or a second-degree relative aged ≤50 years.
- If total cholesterol >9.0 mmol/L even without a family history of CVD.
- Patients with markedly raised triglycerides:
- If triglycerides are persistently >10 mmol/L, despite addressing secondary causes (e.g., poor diet, obesity, diabetes, alcohol excess, medicines). An urgent referral should be made if triglycerides are >20 mmol/L due to the increased risk of acute pancreatitis.
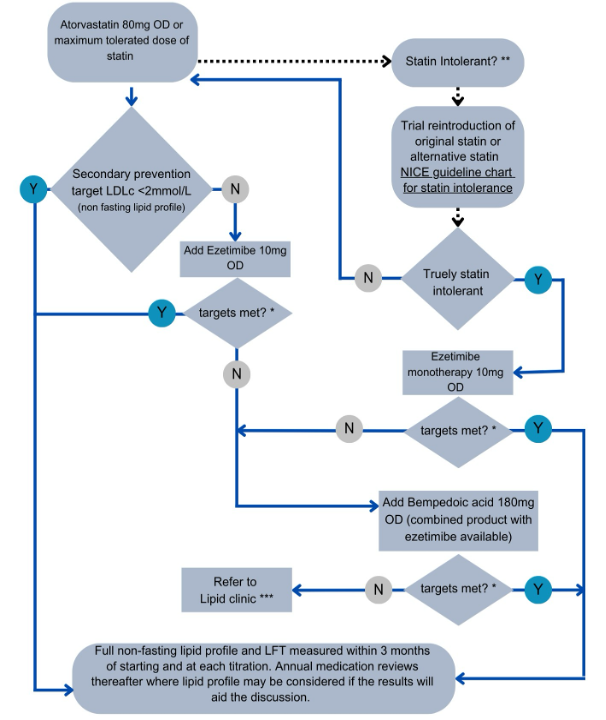
- Patients who fail to meet cholesterol targets after the maximum tolerated dose of statins and other lipid-lowering therapies (e.g. Ezetimibe and Bempedoic Acid) as per the secondary prevention treatment pathway.