This document does not replace current clinical guidance and should be read alongside SIGN 116 and 154.1
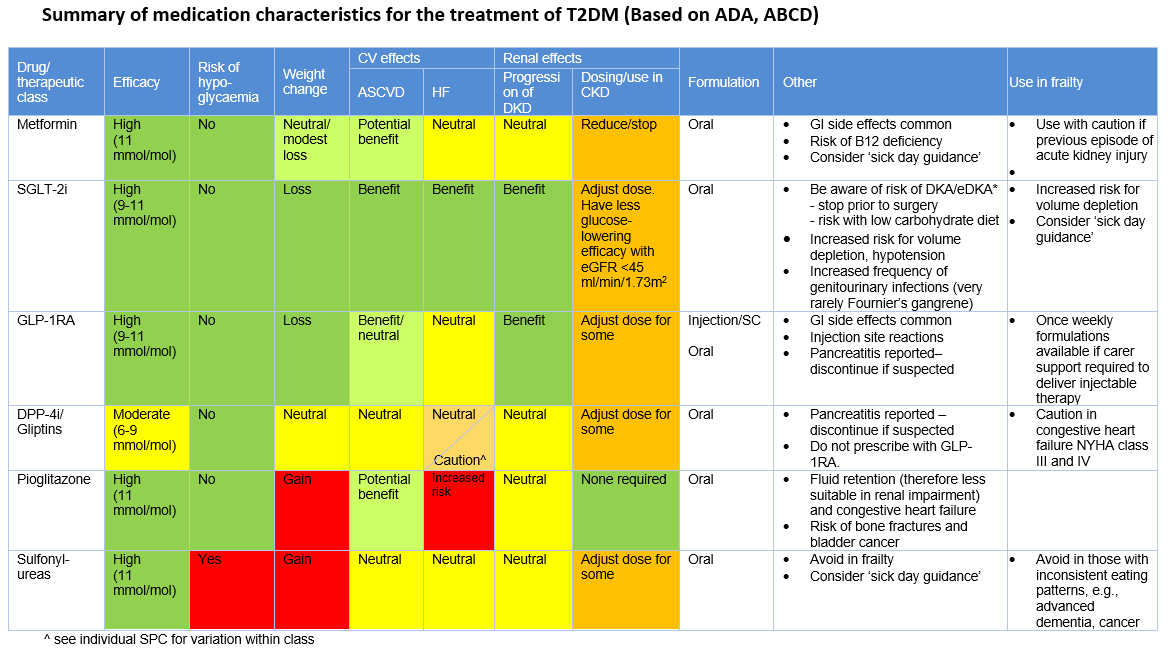
The expert working group also considered the increasing evidence for newer therapies, sodium-glucose co-transporter-2 inhibitor (SGLT-2i) and glucagon-like peptide 1 receptor agonist (GLP-1RA), since publication of the SIGN guidance and the inclusion of these therapies in other national guidelines (such as NICE2 and ADA3). The expert working group considered the place of these therapies in NHS Scotland, recommending their use.