- Mild croup tends to be self-limiting, even without treatment, with shorter time to resolution with dexamethasone treatment.
- In most cases of moderate croup, the symptoms resolve without significant complications.
- With dexamethasone and nebulised epinephrine combination treatment, the prognosis for severe croup is excellent.
- Severe upper airway obstruction can, rarely, lead to respiratory failure and arrest. In children with impending respiratory failure, intubation is required in 1% to 3% of cases. (1)
- Death from croup is rare, occurring in no more than 1 in every 30,000 cases. (3)
Croup (Paediatric Guidelines)

What is Croup?
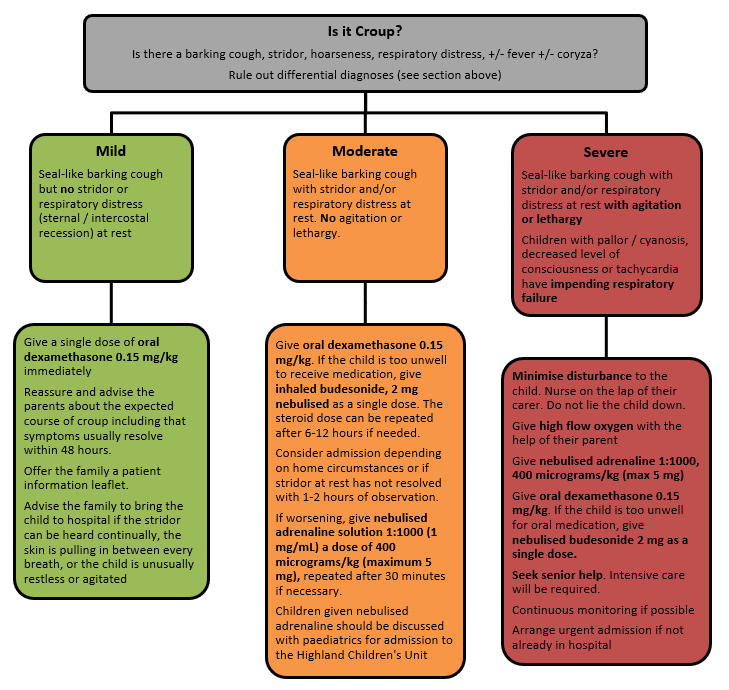
Croup (Laryngotracheobronchitis) is a common childhood respiratory illness characterised by sudden onset of a seal-like barking cough, often accompanied by stridor, voice hoarseness, and respiratory distress. The symptoms are a result of inflammation and narrowing of the subglottic region of the larynx, as a result of viral infection (Typically parainfluenza virus types 1 or 3). (1)
It most commonly affects children between 6 months and 6 years of age, with a peak incidence during the second year of life. Boys are slightly more commonly affected than girls, with a ratio of around 1.4 to 1. (2)
The following clinical signs (In varying combination) are found in croup:
- Stridor
- Seal-like barking cough
- Hoarseness
- Respiratory distress +/- Fever +/- Coryza
The symptoms are typically worse at night and increase with agitation. A minimally invasive hands-off approach allows for the best initial assessment, as children can look very different if allowed to settle for a few minutes. (4)
When seeing an unwell child with cough and stridor, it is important to consider the differential diagnoses, which include:
- Acute foreign body aspiration:
Suspect in a person with sudden onset dyspnoea and stridor, usually a clear history of foreign body inhalation or ingestion, no prodrome or symptoms of viral illness, and no fever (unless secondary infection). - Acute anaphylaxis:
Suspect in a person with acute swelling of the upper airway that may cause dyspnoea and stridor. Fever is uncommon. Swelling of face, tongue, or pharynx may be present. Can occur at any age. - Bacterial upper airway infections: eg. epiglottitis, bacterial tracheitis.
- Bacterial tracheitis is an infection of the tracheal mucosa (usually Staphylococcus aureus or Streptococci) which results in copious secretions and mucosal necrosis. The child often appears very unwell (they look septic, or ‘toxic’) with high fever, croupy cough and signs of progressive upper airway obstruction. The croupy cough and absence of drooling help to distinguish from epiglottitis. Treatment involves securing the airway (over 80% of children with this condition will need intubation) and IV antibiotics (cefotaxime and flucloxacillin).
- Epiglottitis is caused by Haemophilus influenzae B (Reduced incidence after Hib vaccine) or Streptococcus pneumoniae infection, with resultant intense swelling of the epiglottis and surrounding tissues leading to airway obstruction. The onset is usually acute with a few hours of high fever, lethargy, soft inspiratory stridor and rapidly worsening respiratory distress. Cough is usually minimal or absent. The child appears toxic with a high fever and is often sitting immobile with their chin slightly lifted and mouth open drooling saliva. Attempts to lie the child down or painful procedures can precipitate complete upper airway obstruction and so should ideally only be done when the airway has been secured. Treatment involves urgent PICU review for airway assessment and management, bloods for culture and IV Cefotaxime.
Table 1 Differentiation between croup, tracheitis and epiglottitis
Croup | Tracheitis | Epiglottitis | |
Cause | Viral | Staphyloccocus aureus | Haemophilus influenzae B |
Age | 6m to 6yr | Any age | 2 to 6 yr |
Onset | Gradual | Gradual | Sudden |
Pyrexia | Mild | Over 38oC | Over 38oC |
Abnormal sounds | Barking cough, stridor | Barking cough, stridor | Muffled, gutteral cough |
Swallowing | Normal | Difficult | Very difficult with drooling |
Posture | Recumbent | Sitting | Tripod position |
Facies | Normal | Anxious | Anxious, distressed, toxaemic |
Notes
- Dexamethasone tablets can be dispersed in 10mL of water for ease of administration in children. Place the tablet in an oral syringe and draw up 10mL water. Allow to disperse and administer.
- Dexamethasone oral solution (2mg/5mL) (non-formulary) can be used to make up doses that are not whole tablet equivalents.
- If for any reason dexamethasone is not available – use prednisolone 1mg/kg once daily for 2 days. (5)
- A single dose of Prednisolone (1mg/kg) is not as effective as a single dose of dexamethasone for the treatment of croup. Therefore, if using prednisolone as treatment for croup, a second dose is recommended.
- If prednisolone is already given by GP and child has mild croup in Emergency Dept (ED) may not need second dose, but if child has signs of moderate croup consider giving second dose prednisolone 1mg/kg.
- In Raigmore, children with features of severe croup should be reviewed in resus by the paediatric registrar or paediatric consultant before admission to the HCU
- Children with impending respiratory failure should be reviewed by anaesthetics and the paediatric consultant
- Admit children with moderate illness who, after a period of 1 to 2 hours observation after dexamethasone, still have increased work of breathing or stridor at rest
- Hospital admission should also be considered for children with a respiratory rate of over 60 breaths/minute or who have a high fever or 'toxic' appearance
- Children with mild illness may require admission if they have factors that warrant a lower threshold for admission, such as:
- Chronic lung disease
- Haemodynamically significant congenital heart disease
- Neuromuscular disorders
- Immunodeficiency
- Inadequate fluid intake (50 to 75% of usual volume, or no wet nappy for 12 hours).
- Factors that might affect a carer's ability to look after a child with croup, such as
- adverse social circumstances, or
- concerns about the skill and confidence of the carer in looking after a child with croup at home, or the carer being able to spot deteriorating symptoms.
Living a long distance from the hospital (2)
- BMJ Best Practice (2017) Croup. Available from: https://bestpractice.bmj.com/info (accessed February 2021)
- National Institute for Health and Care Excellence (2019) Croup (Clinical Knowledge Summary). Available from: https://cks.nice.org.uk/ (accessed February 2021)
- Bjornson CL, Johnson DW. Croup in children. CMAJ. 2013;185(15):1317-1323. doi:10.1503/cmaj.121645
- NHSGGC Paediatric Clinical Guidelines. Croup. Available from: https://www.clinicalguidelines.scot.nhs.uk/ (accessed February 2021)
- Connie Y. Kuo and Sanjay R. Parikh. Bacterial Tracheitis. Pediatrics in Review. November 2014, 35 (11) 497-499; DOI: https://doi.org/10.1542/pir.35-11-497
| Abbreviation | Meaning |
| ED | Emergency Department |
| HCU | High Care Unit |
| PICU | Paediatric Intensive Care Unit |
