DBS advice
Deep Brain Stimulators are used in people with Parkinson’s and sometimes severe tremors. MRI scan is contraindicated. Monopolar diathermy has been used with caution in patients with a DBS implanted – see manufacturer’s advice. (Heating of electrodes may occur and has resulted in 2 documented cases of severe neurological damage with coma.)
Apomorphine advice
Apomorphine is a potent dopamine agonist given by subcutaneous injection. There are small numbers of people where it is prescribed either in bolus form or with a pump. It is not normally used in the short term as a replacement therapy. Seek advice from relevant Parkinson’s team regarding this.
Duodopa®
Intrajejunal levodopa infusion – frequent difficulties with equipment failure/tube dislodged. Continue at prescribed rate providing gastric emptying is not delayed and the PEJ tube is patent.. Individual patients should have their own protocols for conversion to oral medications.
Other complications associated with Parkinson’s
Falls relate to many issues including postural instability, freezing, postural hypotension, OA , cognitive deficits. Physiotherapy input is important; walking aids may or may not be relevant.
Neuroleptic malignant syndrome may occur on withdrawal of medication, or if medication missed. It can present with delirium, (either hyper or hypo-active) rigidity, fever, and dysautonomia (tachycardia, fever, hypertension or labile BP, sweating) elevated CK; it can be fatal.
Dyskinesia: this may be normal for patient, it may indicate that they are receiving higher doses of medication than normal, or absorption of medicines is different.
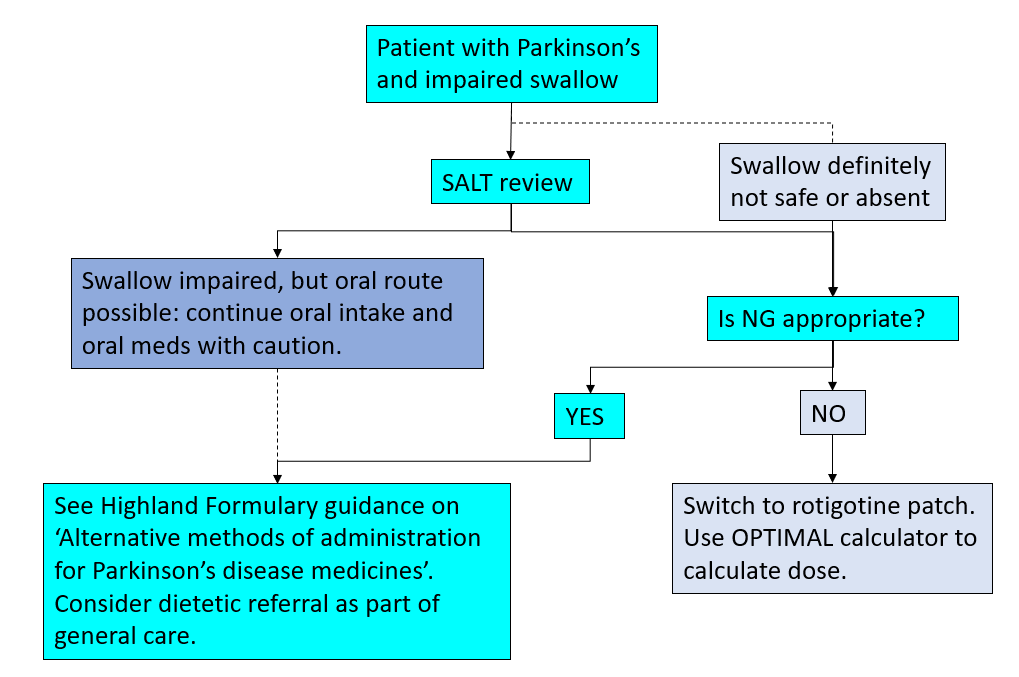
For Parkinson’s patients who have impaired oral intake
Patients who are unwell may be deemed ‘nil by mouth’ if awaiting surgery or investigations, or their swallow may not be effective due to their Parkinson’s, an acute illness or general weakness and frailty.
Appropriate referrals should be made to the SALT and Dietetics teams
Every effort should be made to ensure that Parkinson’s medicines are NOT stopped abruptly.
Advice is given below as to:
- how to switch from oral tablets or capsules, to dispersible forms of levodopa to be administered via nasogastric tube.
- how and when to convert to a transdermal dopamine agonist patch.
- which medications are suitable to be given via a nasogastric tube, see Alternative methods of administration for Parkinson’s disease medicines.
Any patients undergoing a switch away from their normal medication should be referred to the relevant Parkinson’s team for review within one working day of admission – see below for contact details:
Parkinson’s Nurse Specialist ext 6378, Medicine for Elderly ext 5471/5751 or Neurology Secretaries ext 6229/6613.