You have been given this leaflet because you have symptoms of lymphoedema.
What is lymphoedema?
Lymphoedema is a type of swelling. It develops when fluid does not drain easily from areas of the body through the lymphatic system. The lymphatic system normally helps to ensure a healthy balance of fluid in the body. It also deals with infections. Lymphoedema has various causes, and can be a long-term effect of cancer treatment.
How does lymphoedema affect people?
Swelling may be mild, and vary throughout the day. In some people, lymphoedema becomes more of a problem. It can affect the whole arm, hand, breast and/or torso. It may lead to skin changes, sensations of heaviness, and a risk of infection (cellulitis).
What can be done to improve lymphoedema?
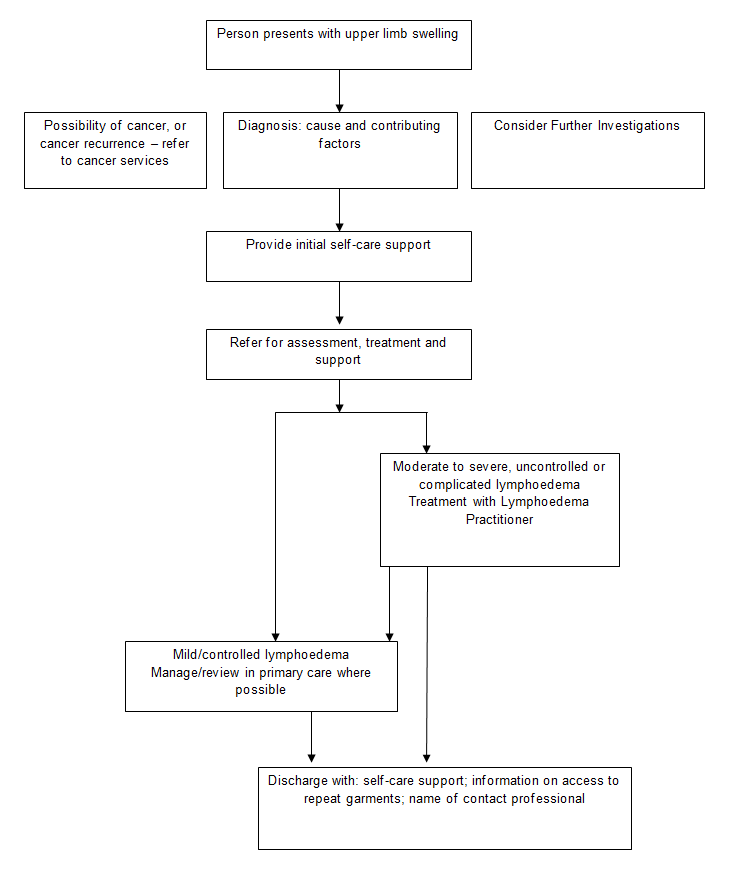
Lymphoedema can be a distressing problem, but with the correct advice and treatment, it can be well controlled. Treatments for arm lymphoedema usually include use of a compression garment to reduce the swelling. Your doctor may refer you for assessment and treatment with a lymphoedema practitioner.
What can I do to manage my lymphoedema?
You can take an active role by following these lymphoedema self-management tips:
Skin care:
- Wash and moisturise your skin daily to keep your skin healthy and supple
- Protect your skin from damage that may lead to more swelling: use insect repellent to avoid insect bites; wear gloves when gardening; protect from sunburn; avoid having your blood pressure taken or injections on the arm
- Use antiseptic cream or spray on any breaks in your skin on the affected area
- If you are unwell, and your arm is red, sore, or more swollen, see your doctor or call NHS 24 immediately as you may have an infection (cellulitis)
Movement and exercise:
- Keep moving your arm as normally as possible, but avoid repetitive movements, and lifting heavy weights; gradually build up the strength in your arm
- Wear a compression garment, particularly while exercising; take it back for more advice if it does not fit.
There may be a lymphoedema group or lymphoedema professional in your area. Ask for more information through your GP surgery or hospital team.