Termination of Pregnancy (Guidelines)

Please note: This guidance has now been updated to come into line with COVID-19; the new, draft guidance, awaiting approval from CEG, is available in the COVID-19 section
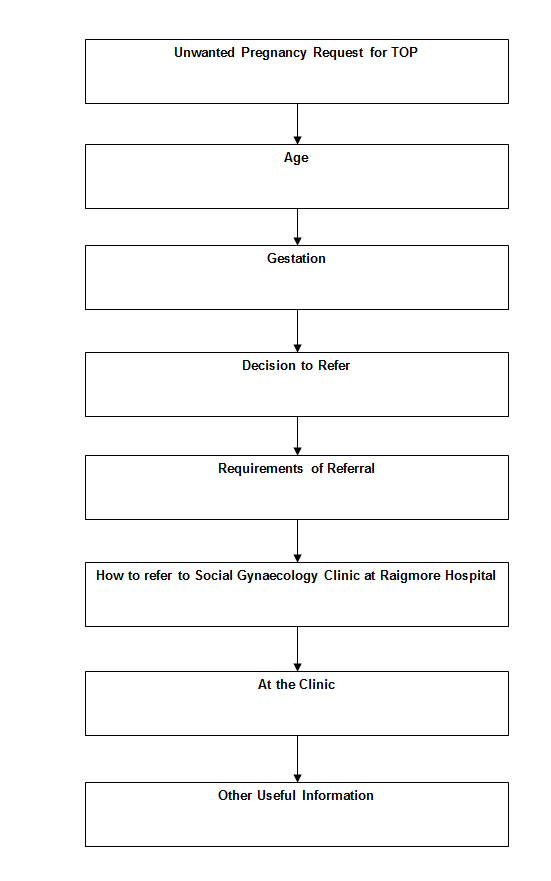
The upper limit for termination of pregnancy locally is 20 weeks. We are happy to see and assess women over 20 weeks, but they will be referred on to BPAS (British Pregnancy Advisory Service) for a termination up to 24 weeks.
If there is any doubt about dates, or you have a patient with a late gestation (16+ weeks), please discuss by telephone where possible (either Social Gynaecology team 01463 704431 or clinic staff 01463 705555 or Dr Hunter’s secretary 01463705289).
Referrals for patients for termination of pregnancy should be made to this service via SCI Gateway. A certificate A (green form) MUST be sent via SCI Gateway with the referral unless there is conscientious objection. Women will not be seen until the pregnancy is at least 5 weeks gestation. SGRS booking operates Monday to Friday from 9am-5pm, excluding public holidays. Clinics are held on Tuesday afternoons and Wednesday mornings.
If you require a telephone consultation for the patient, please ask patient centred booking but usually this is only appropriate for the Western Isles.
Palpate Abdomen
We would be grateful if you could do this to ensure the uterus cannot be palpated. If the uterus is palpable and you cannot get an appointment within 2 weeks, referrals should be discussed by telephone (either Social Gynaecology team 01463 704431 or clinic staff 01463 705555 or Dr Hunter’s secretary 01463705289).
SERVICES | The Social Gynaecology Referral Service (SGRS) is based at Raigmore Hospital, Inverness. Referrals for patients for termination of pregnancy should be made to this service via SCI Gateway. |
WHO TO REFER | GPs and/or other authorities can refer any patient who is having doubts about an ongoing pregnancy. Late Gestation referrals (16 weeks+) should be discussed by telephone (either Social Gynaecology team 01463 704431 or clinic staff 01463 705555 or Dr Hunter’s secretary 01463705289). |
WHO NOT TO REFER | Suspected acute problems should be discussed with the on-call team for Obstetrics and Gynaecology. |
HOW TO REFER | PLEASE USE THE SCI GATEWAY All referrals must be made using the Gateway, launched via the GP application system. Referrals received by 1pm will be processed the same day, those received after 1pm will be processed the next working day. The practice will be notified of the appointment between 2 pm and 4.30 pm on the day the referral is processed. Very urgent referrals should be discussed by telephone with the clinic as above. As SGRS will notify the referring practice by the end of the working day (4.30pm), practices should make arrangements for contacting the patient at this time, as the appointment may be early the next day. Arrangements for the patient to collect the completed Certificate A may also be made. Please ensure that the department is informed of any special requirements, such as interpreters, or unsuitable dates for attendance due to other commitments.The procedure is NEVER performed on the day of clinic attendance. |
FURTHER CONTACTS AND INFORMATION | Urgent contact can be made by calling the above numbers or 01463 705289 |
The appointment takes about 1 hour and the patient is asked to attend with a full bladder. We suggest that she may wish to bring a close friend or relative with her but initially the patient will be seen alone. Children should not attend the clinic appointment.
What happens at the clinic:
- counselling/medical history
- scan to exclude miscarriage, ectopic, molar or multiple pregnancy
- chlamydia & gonorrhoea screening is performed by a self taken swab and women will be offered blood borne virus STI screening
- testing of blood group
- discussion of options including continuing with pregnancy, adoption and TOP
- patient choice is important
- written info is given
- medical TOP offered to all until 20 weeks locally
- surgical TOP possible between 7 - 12 weeks
- those who live locally and fulfil strict criteria (under 9 weeks) are offered early medical abortion at home (EMAH).
- A surgical procedure under local anaesthetic (MVA) is currently not available but will be offered to selected women under 9 weeks in the future.
- We do not offer a "One Stop" service but do keep a space for anyone who requires a termination procedure from further away or for those who are further on in pregnancy. If having a medical termination, they can have their first tablet (Mifepristone) at the clinic. We also have local arrangements to administer Mifepristone in some peripheral hospitals (Caithness and Belford).
- Those who live more than 90 minutes away will not be offered an early medical abortion at home procedure.
- Admission will be arranged within a week for the majority. Because there is such a short time between clinic and admission, a letter from the clinic will only be written when management is not straightforward.
- Please advise the patient that the termination will NOT be done on the day of appointment.
Please inform the patient that the procedure will not be done at the first appointment.
- All women are counselled for contraception at the clinic
- Women are offered a follow up appointment at the Gynae Contraception Clinic if they wish
- If she plans to start contraceptive pills or the patch, we will give her an initial 3 month supply and would be grateful for her GP to prescribe ongoing contraception.
- Depo-Provera can be given before discharge and followed up with her GP.
- Nexplanon can sometimes be inserted at time of admission on the ward.
- At surgical procedures we will insert an IUS/IUD or a Nexplanon if requested.
- Alternatively, the patient can choose to attend the Gynae Contraception Clinic for an insertion of an IUCD or Nexplanon
- Sterilisation cannot be performed at the same time as termination - both for technical reasons and an increased failure rate. A GOPD appointment will be arranged or she will be asked to contact Highland Sexual Health for counselling.
SERVICES | The Social Gynaecology Referral Service (SGRS) is based at Raigmore Hospital, Inverness. Referrals for patients for termination of pregnancy should be made to this service via SCI Gateway. A certificate A (green form) MUST be sent via SCI Gateway with referral unless there is conscientious objection. |
WHO TO REFER | GPs and/or other authorities can refer any patient who is having doubts about an ongoing pregnancy. Late Gestation referrals (16 weeks+) should be discussed by telephone (either Social Gynaecology team 01463 704431 or clinic staff 01463 705555 or Dr Hunter’s secretary 01463 705289). |
WHO NOT TO REFER | Suspected acute problems should be discussed with the on-call team for Obstetrics and Gynaecology. |
HOW TO REFER | PLEASE USE THE SCI GATEWAY |
FURTHER CONTACTS AND INFORMATION | Urgent contact can be made by calling the above numbers or 01463 705289. |
How to refer patients
The Social Gynaecology Referral Service (SGRS) is based at Raigmore Hospital, Inverness. Referrals for patients for Termination of Pregnancy should be made to this service via SCI Gateway. A certificate A (green form) MUST be sent via SCI Gateway with referral unless there is conscientious objection. Women will not be seen until the pregnancy is at least 5 weeks gestation. This is because prior to this point an intrauterine gestation CANNOT be confirmed.
Patient focused booking operates Monday to Friday from 9am-5pm, excluding public holidays. Clinics are held on Tuesday afternoons and Wednesday mornings. GPs and/or other authorities can refer any patient who is having doubts about an ongoing pregnancy Suspected acute problems should be discussed with the on-call team for Obstetrics and Gynaecology. Late Gestation referrals (16 weeks+) should be discussed by telephone and referred using SGRS (either Social Gynaecology team 01463 704431 or clinic staff 01463 705555 or Dr Hunter’s secretary 01463705289).
PLEASE USE THE SCI GATEWAY
All referrals must be made using the Gateway, launched via the GP application system. Referrals received by 1pm will be processed the same day, those received after 1pm will be processed the next working day. The practice will be notified of the appointment between 2pm and 4.30pm on the day the referral is processed. Very urgent referrals should be discussed by telephone with the clinic as above. Patient focused booking will notify the referring practice by the end of the working day (4.30pm), practices should make arrangements for contacting the patient at this time, as the appointment may be early the next day. Arrangements for the patient to collect the completed Certificate A may also be made. Please ensure that the department is informed of any special requirements, such as interpreters, or unsuitable dates for attendance due to other commitments. The procedure is NEVER performed on the day of clinic attendance.
PATIENTS MAY CONTINUE TO SELF-REFER BY USING THE APPOINTMENTS NUMBER ON 01463 705667 (a patient booking number is NOT required for this).
Where are women requesting TOP seen?
We have a specially run Social Gynaecology clinic at Raigmore Hospital which operates once a week on a Wednesday morning and a Tuesday afternoon.
We DO NOT offer a “one stop” service but do keep a space for anyone who requires a termination procedure from further away or for those who are further on in pregnancy so that there is minimal delay and/or travel for the patient.
Can they have a telephone consultation?
Phone 01463 705667 and ask but this is mainly reserved for those from the Western Isles and Caithness.
What is the “cut off” point?
20 weeks is our cut off point. If there is any doubt about dates, or you suspect late gestation (16 weeks+) or she has a palpable uterus, then please state this clearly to the appointments office who will highlight this to a professional. Patients who exceed 20 weeks can be assessed at BPAS in Glasgow, but will have to go to England for completion of the procedure. Regardless of gestation, the patient should always be seen initially at the clinic for discussion and dating scan. NHS Highland will fund this. BPAS contact details are:www.bpas.org.uk phone number 03457 304030.
Under 16’s
In keeping with the Fraser Guidelines, those under 16 years of age can consent to the procedure as long as there is no element of coercion suspected. We do, however, encourage them to involve an adult, if not their parents. We adhere to local child protection guidelines.
What if she is undecided?
We are happy to see women that are undecided and will review those who need more time to fully make up their mind one way or another.
Do I get a clinic letter?
Admission will be arranged within a week for the majority. Due to there being such a short time between clinic and admission, a letter will only be written when management is not straightforward. You will be informed via the Social Gynaecology Nurse of any women who do not attend.
Post-Procedure contraception
Women are encouraged to attend their GP/source of referral for a follow up to ensure no complications and that they have adequate contraception. If your patient’s plans are to start pills or the patch, we will provide an initial 3 month supply and would be grateful if you could supply ongoing contraception.
LARC methods (Depo-Provera, Nexplanon and IUCDs) may be initiated/inserted prior to discharge. At surgical procedures we will insert an IUS/IUD or Nexplanon if requested. All women are offered a follow up appointment at the Gynae Contraception Clinic for ongoing contraception, including insertion of an IUS/IUD or Nexplanon.
Sterilisation cannot be performed at the same time as termination – both for technical reasons and an increased failure rate. A further appointment is required.
| Abbreviation | Meaning |
| TOP | Termination of pregnancy |
| STI | Sexually transmitted infection |
| IUS/IUD | Intrauterine system/intrauterine device |
| GOPD | Gynaecology outpatient department |
