Risks associated with NG Tube insertion
NG tube feeding is common in all groups of people from neonates to older people and most tubes are inserted without incident, however there is a small risk that misplacement into the lungs instead of the stomach can be fatal. The National Patient Safety Agency (NPSA 2011) Scottish Government Safety Action Notice SAN (SC) 16/03 (2016) provides guidance on a number of safety critical requirements which are reflected within this policy.
Risks associated with NJ Tube insertion
Nasojejunal tubes are principally used in individuals with delayed gastric emptying and are often employed for nutrition support when their problems are long-standing. Under these circumstances, it is usually adequate to recommend a prolonged fast prior to endoscopy and NJ tube insertion. For in-patients who may have an acute cause of gastric stasis but are suitable for NJ feeding (most commonly in those with acute severe pancreatitis) it is imperative that the stomach is adequately drained with a wide-bore NG tube prior to endoscopy as there is a significant risk of aspiration of large volumes of gastric contents at the time of gastroscopy which in turn can be associated with pneumonia, pneumonitis or death.
NG Tube Insertion & Checking
All staff responsible for insertion and checking placement of nasogastric tubes (including staff supporting parents/carers who check initial placement of nasogastric tubes) must have successfully completed both theoretical and competency-based assessment for NG tube insertion and care. Unless clinically urgent, if there is insufficient experienced staff to accurately confirm nasogastric tube placement (for example at night), then placement should be delayed until support is available. The rationale for any decisions made must be recorded in the person’s medical notes.
For details of how to access NHS Highland staff training please see Resources / Key Contacts.
The position of the NG tube must be checked following initial placement and before anything is introduced via the NG tube.
- pH checking should be used as the first line test method
- Check NG tube placement using pH indicator strips CE marked for human aspirate
- Very carefully aspirate fluid from the NG tube by gently pulling back on plunger until a small amount of fluid (at least 0.5 – 1ml) appears in the syringe.
- Test the pH of the aspirated fluid by dripping onto CE marked pH paper
- Cover the 3 small squares of paper with gastric contents.
- The aspirate will react with the paper.
- Match the 3 squares to the scale on the box.
- If the pH is 1-5.5 it is reliable confirmation that the tube is not in the lung (NHS Improvement July 2016) however if the pH reading is between 5-6, a second competent person must confirm the range of 1-5.5.
- If the pH is above 5.5 nothing must be administered via the tube and xray confirmation should take place.
- If aspirate cannot be obtained, try one or more of the following and then repeat the aspiration procedure:
- Use an enteral syringe to insufflate up to 20ml air down the tube to dislodge any debris from the end of the tube and move the tip away from the gastric mucosa
- Where possible ask the patient to move/walk about or move onto right side.
- Where safe to do so ask the patient to take a drink of tap water (do not put down the tube)
- X-ray is used only as a second line test when aspirate cannot be obtained or pH indicator paper has failed to confirm the location of the nasogastric tube.
The following information should be recorded on the NHSHighland Adult NG Tube Insertion Record (Available on PECOS):
- Who confirmed the position of the nasogastric tube (this individual must be evidenced as competent to do so)
- Confirmation that any x-ray viewed was the most current x-ray for the correct patient.
- The rationale for the confirmation of position of the nasogastric tube, i.e. how placement was interpreted and clear instructions as to required actions.
Once the position has been confirmed remove the guide wire carefully and dispose of it in a sharps bin. Tape the tube securely on the nose and cheekbone or forehead using adhesive tape (check patient is not allergic to tape). Mark the tube at the nose with a permanent marker and each time the tube is used check the mark is still in the same place. Tube placement must always be checked before feeding commences and before drug administration and be documented on the NHS Highland Adult NG Tube Position Check & Care Record (Available on PECOS)
If the tube becomes displaced always re-check its position by aspirating prior to the commencement of feeding.
Tubes should be replaced after 28 days or as per manufacturer’s guidelines. It is advisable to use the other nostril where possible as this reduces risk of mucosal irritation.
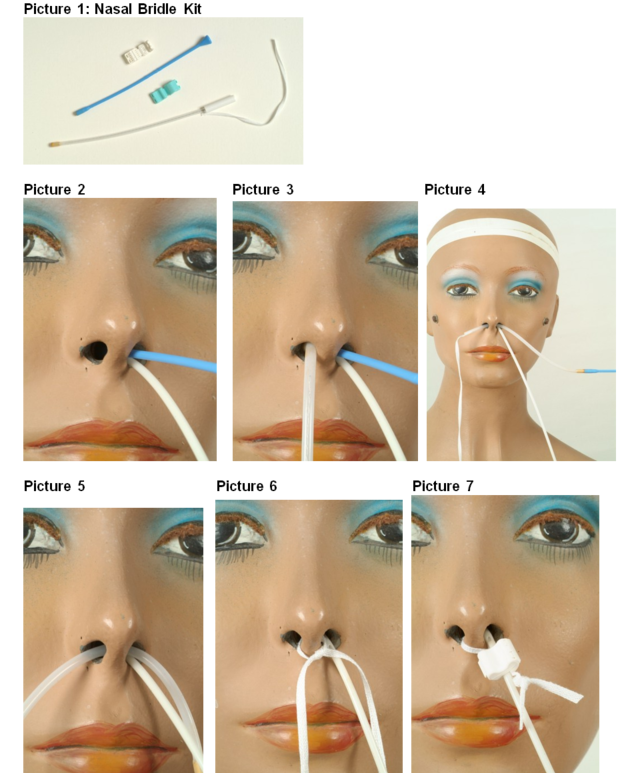
Nasal Bridles
Nasal bridles are a method of preventing inadvertent displacement or removal of fine-bore nasogastric feeding tubes in individuals requiring enteral administration of feed, fluid or medication.
Individuals who could be considered for nasal bridle include:
- Those who have pulled out at least 2 NG tubes
- Those who have experienced the displacement of 2 NG tubes within 48 hours
- Those who experience irritation to the skin as a result of tape and/or liquid adhesives
- Those who require a NJ tube
- Those to be discharged from the acute setting on long term NG tubes
Individuals who should be excluded from nasal bridle placement include:
- Severely agitated people who are deemed likely to traumatise themselves via traction on the tube
- Those with facial or cranial trauma
- Those with basal skull fractures
- Those with severely deviated or obstructed nasal septum or passage
- Those with any structural deformity of the nose, nasopharynx
- Those with nasotracheal tubes
- Those who have received thrombolysis for acute stroke or MI in the last 5 days
- Those on oral anticoagulation medication
For additional guidance please see Pictorial Guide to Nasal Bridle Insertion.
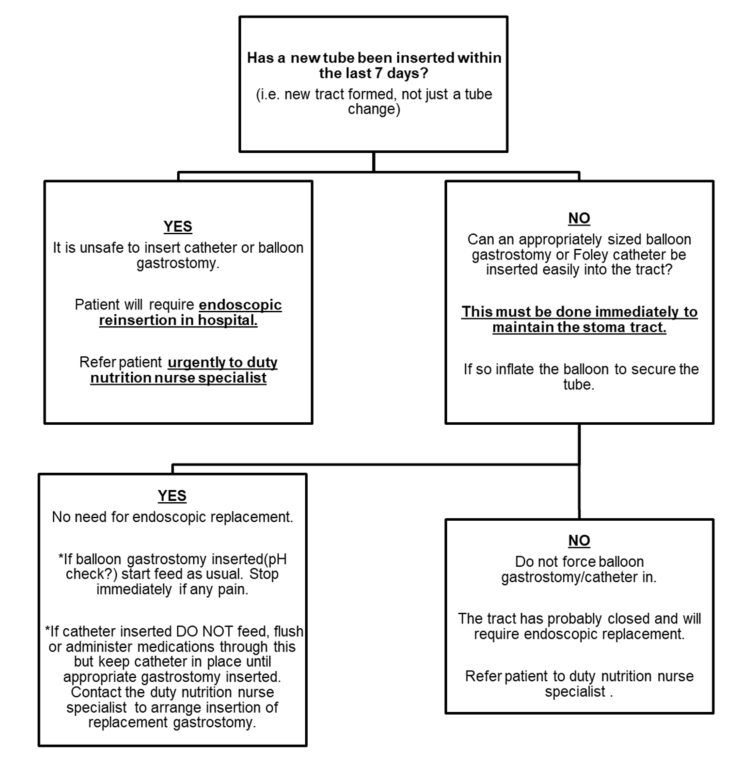
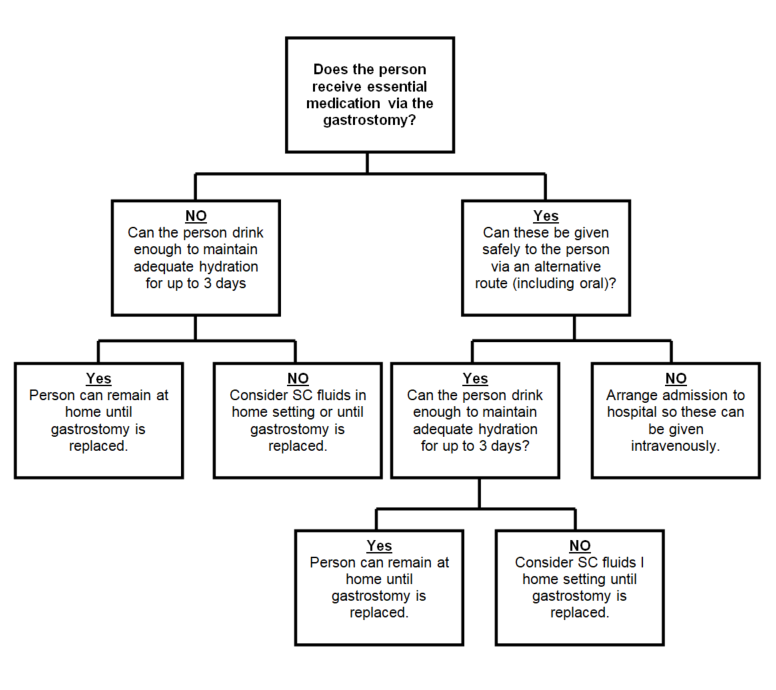
Gastrostomy and Jejunostomy Tube Position
Gastrostomy and jejunostomy tubes are much less likely than NG tubes to become dislodged and it is not necessary to check their position prior to use, however if there appears to be a change in the position of the tube as it enters the abdomen or pain is evident on flushing of the tube, it should not be used until correct position is confirmed – see section on management of displaced feeding tubes. The nutrition nurse specialist or managing healthcare professional should be contacted for advice.
NJ and PEG-J Tube Position
It is not possible to check the position of a jejunal tube using the same methods as a gastric tube as the pH of jejunal contents are not usually acidic. While the gastrostomy component of a PEG-J is unlikely to be dislodged, it is possible for the jejunal inner tube to fall back in to the stomach. The same is true of an NJ tube. If an individual being fed using either of these routes feels nauseous when fed or vomits feed, a dislodged jejunal tube should be suspected and feeding stopped until the feeding tube position can be clarified. The nutrition nurse specialist should be able to help co-ordinate care as it may be necessary to arrange gastroscopy to insert a new NJ tube or re-position the jejunal extension tube.