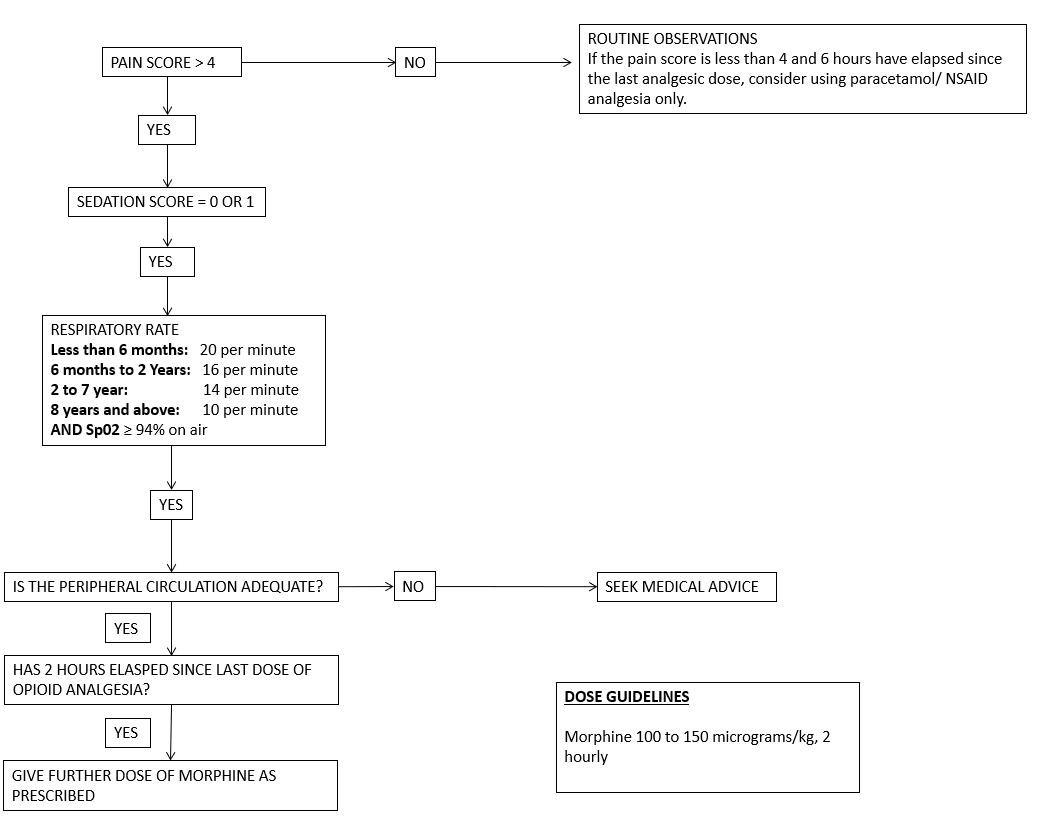
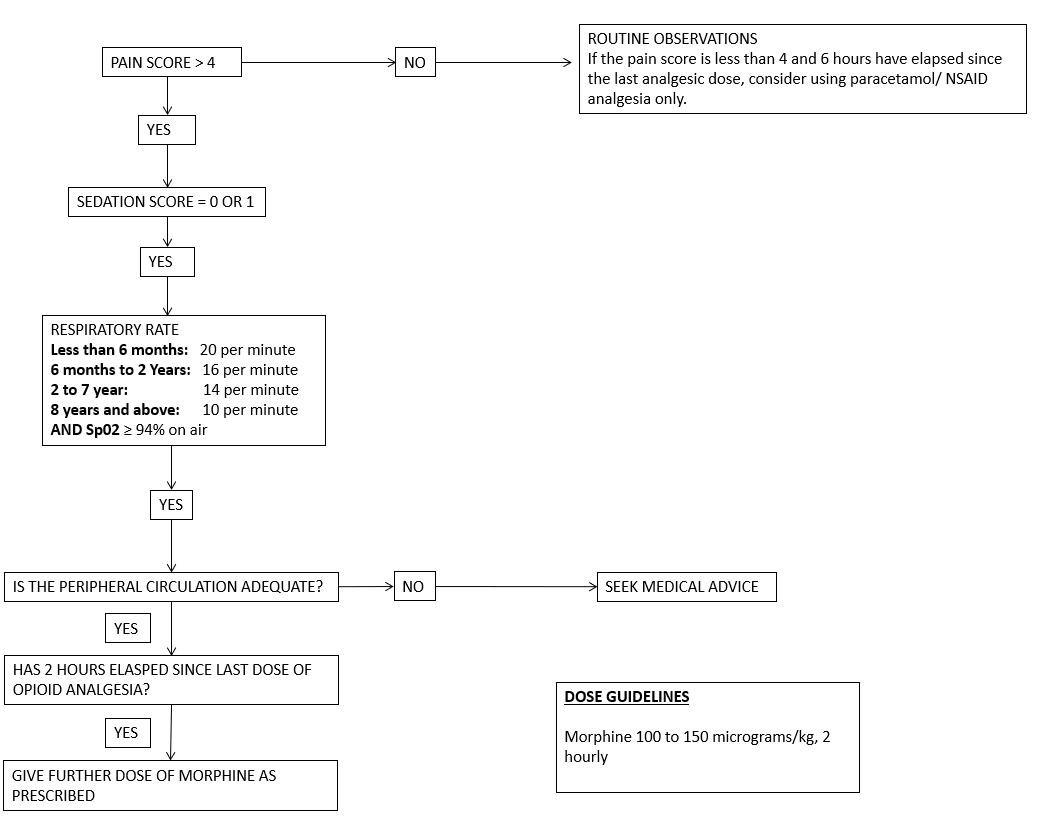
Always use this algorithm prior to administering an opioid

Morphine is the opioid of choice.
Caution should be exercised in the following children, and the opioid dose should be reduced:
The following children are NOT SUITABLE for the opioid algorithm:
All children should have patent intravenous access.
Nursing staff should be competent in the use of the opioid algorithm and have attended In-service training on its use.
All areas must have NALOXONE (0.4mg ampoule) immediately available.
Always use this algorithm prior to administering an opioid
Pulse, oxygen saturation levels, respiratory rate, pain score, sedation score and nausea score must be recorded on the observation chart as follows: