Complications of PCA are related to opioid side effects. NSAIDS and Paracetamol help to minimise side-effects by reducing the total dose of opioid required and work best if administered regularly rather than an “as required” basis.
Naloxone and managing complications of opioids (Paediatric Guidelines)

Warning
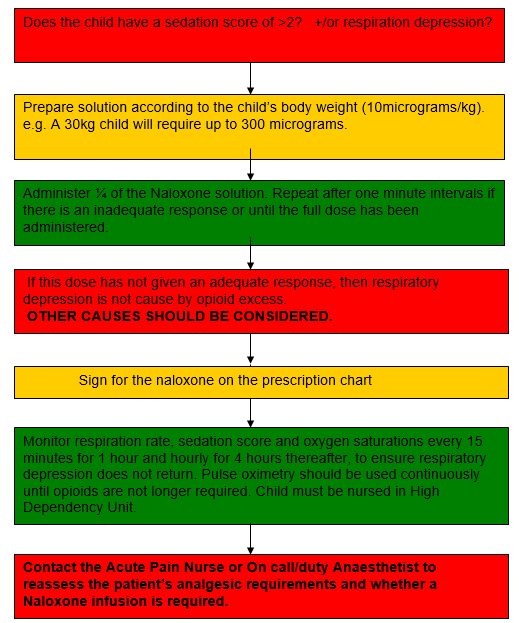
PREPARATION OF NALOXONE
Naloxone must be readily available on all wards where opioids are used. All trained nursing staff should know where it is stored.
- Administer oxygen by facemask and ensure a clear airway.
- Remove the PCA handset or consider stopping/reducing infusion.
- Stay with the child and monitor respiratory rate, sedation and oxygen saturation levels continuously.
- Contact medical staff or On call / duty anaesthetist for further advice.
- Assess for other causes of hypoxia / sedation and treat appropriately.
- Review analgesia with On call / duty anaesthetist or Acute Pain Nurse.
| Age | Breaths per minute |
| Less than 6 months | below 20 breaths per minute |
| 6 months to 2 years | below 16 breaths per minute |
|
2 years to 7 years
|
below 14 breaths per minute
|
| 8 years and over | below 10 breaths per minute |
- Administer oxygen by facemask and ensure a clear airway.
- Remove the PCA handset or stop infusion.
- Stay with the child and monitor respiratory rate, sedation and oxygen saturation levels continuously.
- Contact medical staff or On call / duty anaesthetist for further advice.
- Assess for other causes of hypoxia / sedation and treat appropriately.
- Review analgesia with On call / duty anaesthetist or Acute Pain Nurse.
| Age | Breaths per minute |
| Less than 6 months | below 18 breaths per minute |
| 6 months to 2 years | below 14 breaths per minute |
|
2 years to 7 years
|
below 12 breaths per minute
|
| 8 years and over | below 8 breaths per minute |
- Administer oxygen to maintain spO2 > 95% by facemask and ensure airway is clear.
- Stop the PCA pump and remove the PCA handset.
- Contact the On call/duty anaesthetist urgently.
- Administer naloxone IV (10 micrograms/kg). Give ¼ of the dose and repeat after 1 minute intervals, until the maximum dose has been given. A naloxone infusion may be required.
- If the response to naloxone is inadequate then consider other causes.
- Review analgesia with the On call/duty anaesthetist or Acute Pain Nurse.
- The child must be nursed in the High Dependency Area until PCA or parenteral opioids are no longer required.
- If the child’s sedation score is 3, treat as for severe respiratory depression.
- If it is 2, treat as for moderate respiratory depression.
Side effects of opioid analgesics include sedation and respiratory depression. Sedation usually precedes respiratory depression and is therefore an early indication of potential respiratory depression.
- All children must have their sedation score recorded at the same time as their vital observations using the above scoring tool.
- Only qualified nursing staff may assess children.
- If the child has a sedation score of 2, 1:1 nursing care must be carried out.
- If the sedation score = 3, the following must be carried out immediately:
- Contact a paediatrician and the ITU anaesthetist.
- Administer oxygen via Hudson face mask
- Give naloxone intravenously.
- Stop opioids: i.e. IV infusion, patient controlled analgesia, oral or subcutaneous.
- Contact the Acute Pain Nurse so that we are aware of this patient and can give assistance if required.
Sedation score tool
|
S
|
Normal sleep |
|
0
|
Awake |
|
1
|
Mildly sedated: Awakes to verbal stimuli |
|
2
|
Moderately sedated: Requires verbal AND touch stimuli |
|
3
|
Severely sedated: Unarousable OR difficult to awaken |
- Give prescribed anti-emetic. It may be beneficial to use more than one agent.
- See: Nausea and Vomiting Assessment Tools (Paediatric Guidelines)
- Assess cause - it may not be the opioid.
- Prescribe antihistamine as required - Chlorphenamine.
| Age | Dose |
| 2 to 6 years | 1mg, every 4 to 6 hours. Max 6 mg daily. |
| 6 to 12 years | 2mg every 4 to 6 hours. Max 12mg daily. |
|
12 to 18 years
|
4mg every 4 to 6 hours. Max 24mg daily
|
- Hypotension is not usually due to opiates but may be caused by Hypovolaemia, bleeding, sepsis or anaphylaxis and should be taken seriously.
- Contact ward doctor for advice.
- Mobilise with support at all times.