Gallstone disease pathway
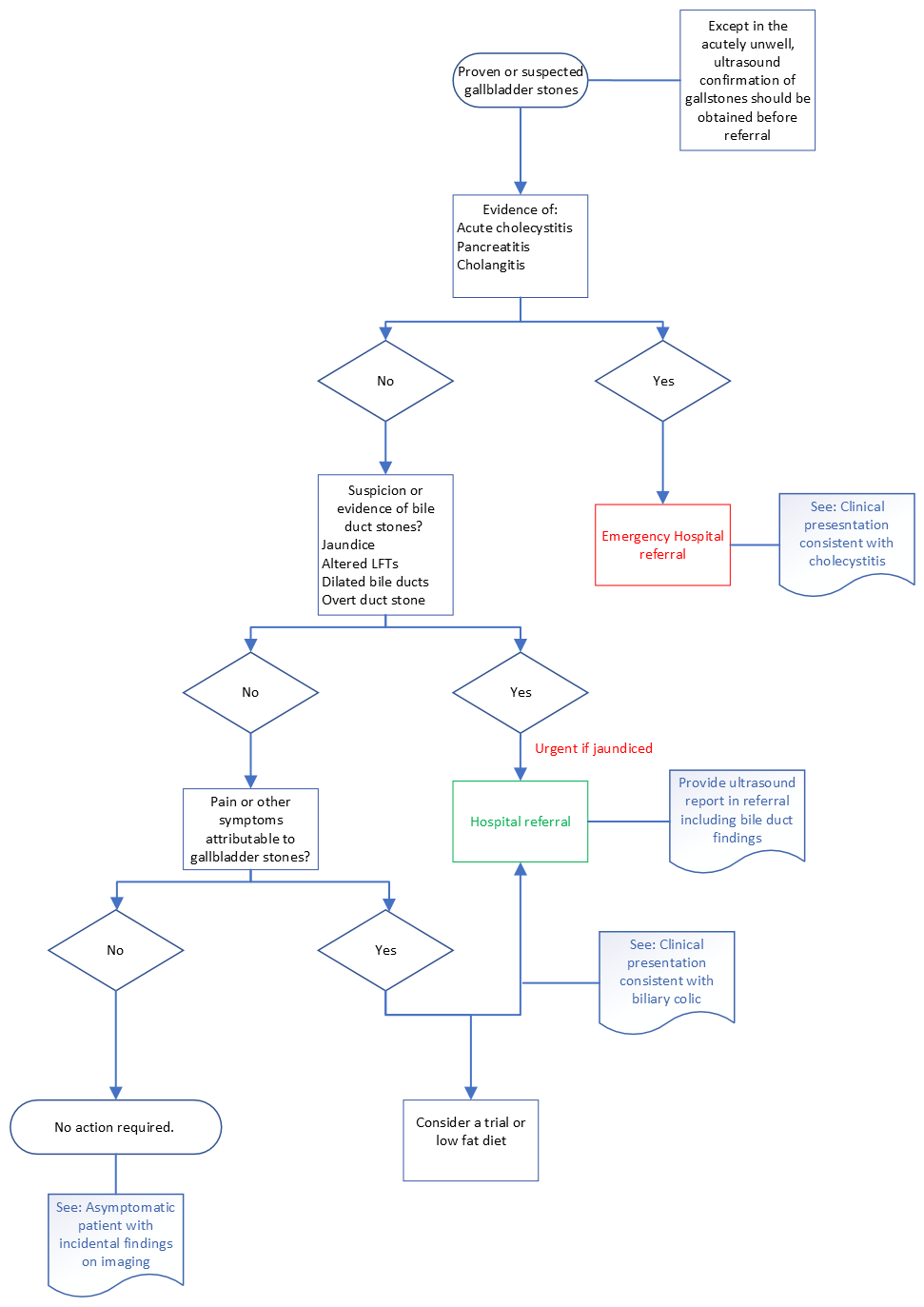
From 2016 RCSEng/AUGIS Commissioning Guide.

10 to 15% of the adult population in the UK have gallstones, the majority of which are asymptomatic and require no treatment.
Presentation of symptomatic gallstones is usually with biliary colic or, less commonly, a complication of gallstone disease, most commonly cholecystitis.
The definitive treatment of symptomatic gallstones is cholecystectomy.
Stones may pass from the gallbladder into the CBD (common bile duct) and present with jaundice, cholangitis, pancreatitis.
Gallstones on abdominal USS
No treatment or referral
CBD stone
Routine referral due to the risk of potentially significant complications.
(If the patient is currently asymptomatic but there has been a history of jaundice or infection consider urgent referral)
Most patients with symptomatic gallstones present with a self-limiting attack of RUQ / epigastric pain, frequently radiating to the back +/- nausea/vomiting.
This can usually be controlled in primary care with appropriate analgesia +/- anti-emetics without hospital admission.
Consider checking LFTs and a routine referral for USS (although may be deferred until symptoms become recurrent – please see below)
When pain cannot be managed or if the patient is otherwise unwell (septic), refer as an emergency to the on-call surgical team
Further episodes of biliary colic are common (50% risk per annum with 1 to 2% risk per annum of complications).
If not done following the initial presentation, arrange for LFTs to be checked and request a routine USS (unless LFTs are significantly abnormal or the patient is clinically jaundiced. (See section: Clinical suspicion of biliary obstruction)
Recurrent episodes can be prevented in around 30% of patients by adopting a low-fat diet (fat in the stomach provokes release of cholecystokinin, which precipitates gallbladder contraction).
If gallstones (including the suggestion of gallbladder sludge) are confirmed on USS, and the patient is considered fit for and would desire surgery, refer routinely for consideration of cholecystectomy
If the gallbladder is normal with no gallstones identified, consider an alternative diagnosis e.g dyspepsia.
There is NO evidence to support the use of:
(with or without known gallstones)
Ideally patient with acute cholecystitis should have a cholecystectomy in the same admission but if the patient is clinically well and admission is not felt to be required based on clinical condition, management of cholecystitis in the community with analgesia and anti-emetics may be appropriate. If in doubt a discussion with the on-call surgical team would be appropriate.
In the case of management in Primary Care
If the patient cannot be managed in the community, refer the patient to the on-call surgeon with view to admission.
(with or without known gallstones)
If there is a clinical suspicion of acute pancreatitits or cholangitis, refer the patient to the on-call surgical team.
Patients with known gallstones and jaundice or clinical suspicion of biliary obstruction (e.g. significantly abnormal LFTs), not requiring same day admission (i.e not septic), should be referred urgently.