 R
R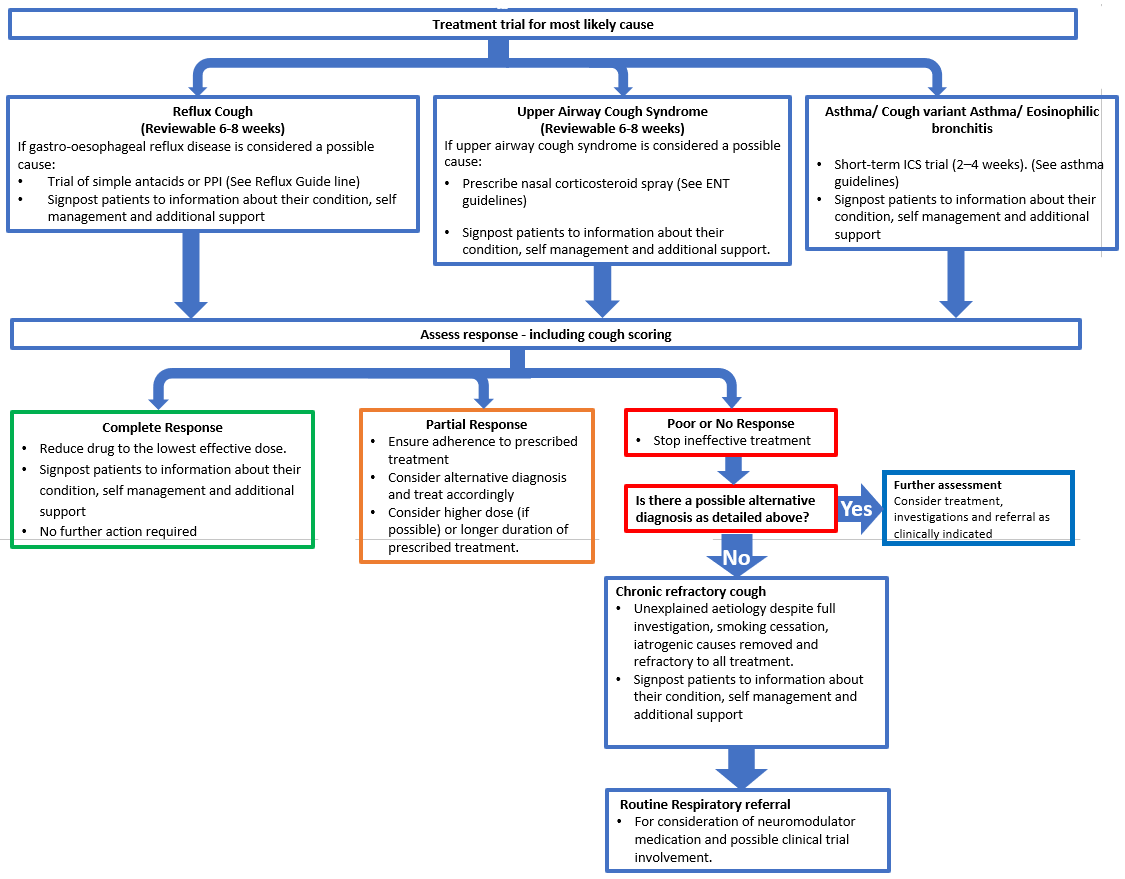
Chronic cough (Guidelines)

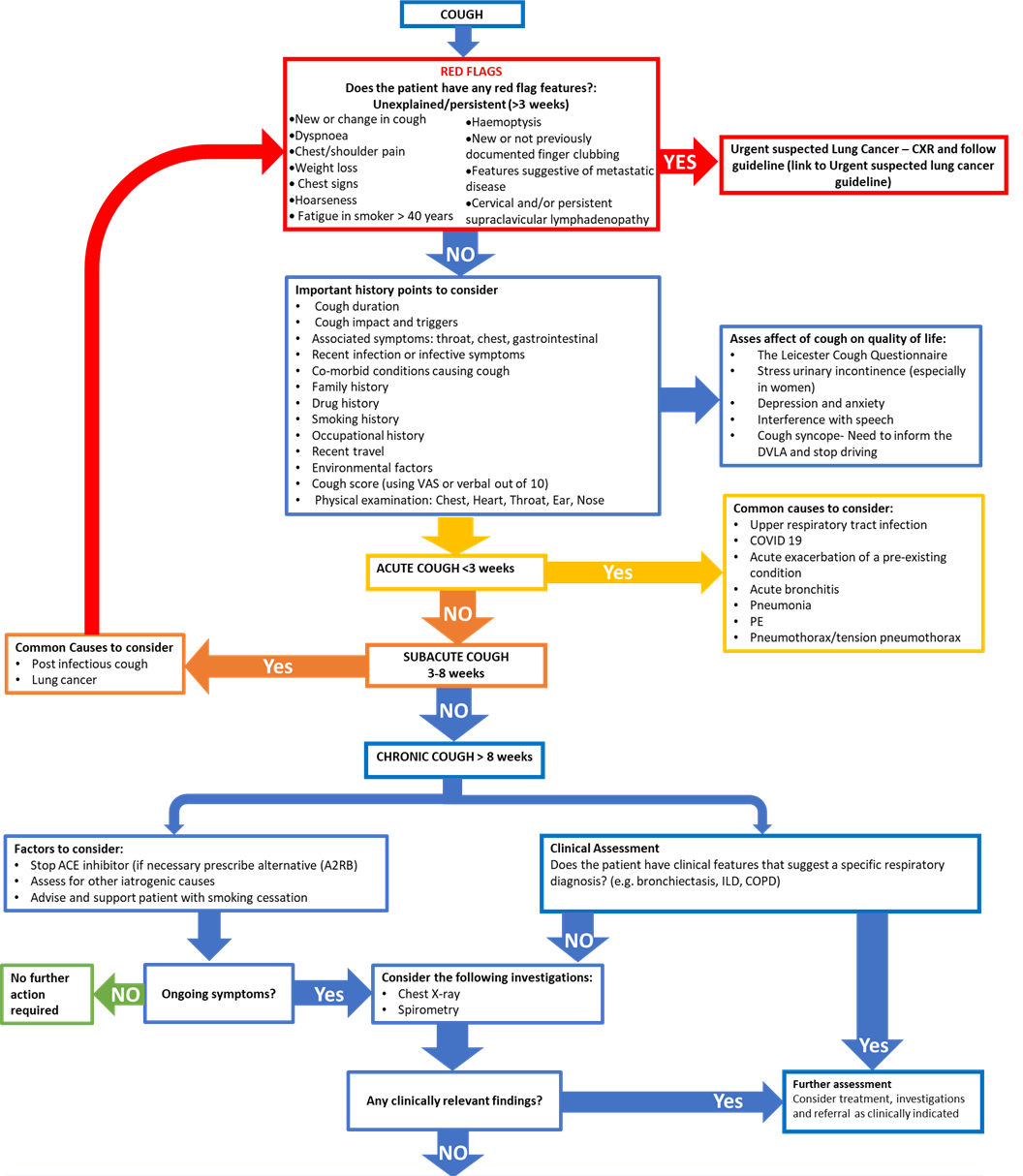
Cough is a vital protective reflex necessary to prevent aspiration and clear the airways of mucous. However excessive and protracted coughing can be very disabling and greatly affect a patient’s quality of life.
It affects an estimated 5 to 10% of adults.
As cough is a common medical symptom which can be associated with a number of different conditions, this guideline aims to aid clinicians in the diagnosis and management of chronic cough.
- Take a comprehensive history including:
- Duration
- Triggers
- Diurnal variability
- Red flag symptoms/features- exclude malignancy
- Associated symptoms – Chest, Throat
- Infective symptoms- Exclude active infection
- Recent respiratory tract infection
- Co-morbid conditions causing cough- exclude exacerbation of known condition
- Gastrointestinal symptoms
- Symptoms of heart failure
- Smoking history
- Occupational history
- Recent travel
- Environmental factors
- Cough scoring – out of 10/ Visual analogue scale
- Drug history – exclude iatrogenic cause
- Assess the effect of the cough on a patient’s quality of life using tools, such as the Leicester Cough Questionnaire: The Leicester Cough Questionnaire and specifically ask about symptoms of:
- Stress urinary incontinence (especially in women)
- Depression and anxiety
- Interference with speech
- Cough syncope- Need to inform the DVLA and stop driving: https://www.gov.uk/guidance/neurological-disorders-assessing-fitness-to-drive
And offer appropriate support and management.
- Exclude the presence of a respiratory condition (infection, COPD, ILD, Asthma etc)
Examination
Complete a thorough examination including
- Chest
- Heart
- Ears
- Pharynx
Investigation
- Spirometry
- CXR
Acute cough- less than 3 weeks
- Defined as a cough which has been present for less than three weeks.
- Most common causes to consider
- Upper respiratory tract infection
- COVID 19
- Acute exacerbation of a pre-existing condition -Asthma, COPD, Bronchiectasis
- Acute bronchitis
- Pneumonia
- If associated with acute onset of breathlessness and chest pain, consider
- PE
- Pneumothorax/tension pneumothorax
Subacute Cough 3 to 8 weeks
- Defined as a cough which has been present for three to eight weeks.
- Most common causes to consider:
- Lung Cancer (especially in current/ex-smokers) -Asses for any Red flag symptoms
- Post infectious cough (eg after Mycoplasma pneumonia or Bordetella pertussis) Persistent dry cough with a history of a recent acute respiratory infection, in a systemically well patient, with a normal examination.
Urgent suspected Cancer
Patients presenting with any of the following red flag symptoms/signs for lung cancer should follow the Urgent Suspected Cancer pathway (link to USC guideline).
- Any unexplained haemoptysis
- New/ not previously documented finger clubbing
- Persistent or recurrent chest infections
- Cervical and/or persistent supraclavicular lymphadenopathy
- Thrombocytosis where symptoms and signs do not suggest other specific cancer
Unexplained and persistent symptoms lasting more than 3 weeks:
- change in cough or new cough
- dyspnoea
- chest/shoulder pain
- loss of appetite
- weight loss
- chest signs
- hoarseness (if no other symptoms present to suggest lung cancer refer via Head & Neck pathway)
- fatigue in a smoker aged over 40 years
Any patient who has consolidation on chest x-ray should have a repeat no more than 6 weeks later to confirm resolution regardless of hospital admission or not if:
- Symptoms/physical signs persist
- There is higher risk of underlying malignancy
- smokers
- aged over 50 years
Chronic Cough greater than 8 weeks duration
- Defined as a cough which has been present for more than eight weeks.
- The most common causes of chronic cough are listed below in Differential diagnosis and management
- Other causes of chronic cough to consider are:
- Infective causes - Pertussis
- Pulmonary tuberculosis
- Respiratory conditions
- COPD
- Asthma
- Interstitial lung disease
- Bronchitis
- Obstructive sleep apnoea – awaking from sleep with cough
- Lung Cancer
- Bronchiectasis
- Other conditions causing cough
- Heart Failure
- Somatic cough syndrome
- Environmental/occupational exposure to a cough trigger
Bronchiectasis
- Bronchiectasis is characterized by permanent, irreversible dilation of the bronchi due to inflamation and damage to the airways.
- Symptoms include intermittent infection and persistent daily expectoration of purulent sputum
- Due to the widening of the airways, mucous is able to accumulate which increases the risk of respiratory infection.
- Because of this, it is beneficial for patients with bronchiectasis to cough regularly to expectorate the sputum and reduce their risk of infection.
- However patients can struggle with regular coughing, particularly if their cough is ineffective and may find it exhausting.
Management
- Sign posting to relevant information about effective cough and airway clearing techniques. (see social prescribing guidance for resources)
Smoking and Nicotine
- Smoking and smoking exposure are a cause of chronic cough
- Always consider COPD and Lung cancer as a cause of cough in a current or ex-smoke
Management
- Refer to the smoking cessation service
- Note- Nicotine is a cough suppressant so patients should be warned that they may experience a transient increase in coughing after quitting smoking.
Asthma
Classic asthma
- Patient has features of bronchoconstriction and bronchial hyperresponsiveness
- Spirometry or peak flow show airflow variability.
Cough variant asthma
- Patient has features of hyperresponsiveness with cough as their main symptom
- Patient may have normal spirometry and lack peak flow variability.
Eosinophilic bronchitis
- A condition characterised by eosinophilia in the airways causing cough.
- Patient presents with cough but no features of bronchoconstriction or hyperresponsiveness
- Patients have normal peak flow and spirometry
Management
- Short-term ICS trial (2 to 4 weeks)
- If patient improves follow asthma guidelines for continued management: Asthma in adults (Guidelines)
- If no improvement, Stop medication and reconsider diagnosis.
Reflux cough
- Reflux cough is characterised by either gastroesopahgeal or oesophagealpharangeal reflux, due to either reflux or dysmotility, causing aspiration resulting in airway inflammation
- This inflammation may be neutrophilic or esinophilic and results in an asthma type cough and excessive mucous production.
- Common symptoms of reflux cough include change in voice, nasal symptoms and dysgeusia.
- Patients may also present with recurrent aspiration pneumonia, bronchitis and bronchiectasis secondary to reflux rather than being the primary cause of the cough.
Management
- Trial of simple antacids and PPI- see upper GI Reflux Guidelines
- If presenting with symptoms of dysmotility such as dysphagia, consider referral to gastroenterology.
Review
- 6 to 8 weeks.
- If improvement, manage as per GI guidelines. No further action required
- If no improvement, Stop medication and reconsider diagnosis.
Upper airways Cough syndrome
- Patient presents with cough associated with symptoms of persistent throat clearing and a feeling of something in the back of the throat, nasal discharge, congestion or recurrent sneezing.
- Cough results from irritation of afferent nerve pathways in the upper airways.
- Often associated with seasonal or occupational triggers
- Can be associated with Reflux or Asthma
Management
- Trial of nasal steroid- See NHSH ENT Guidelines and ENT nasal discharge
Review
- 6 to 8 weeks.
- If improvement, manage as per ENT guidelines. No further action required
- If no improvement, Stop medication and reconsider diagnosis.
Iatrogenic cough
- Cough secondary to medication.
ACE inhibitors
- Can increase the sensitivity of the cough reflex and can cause cough in up to 15% of patients.
- Should not be prescribed in patients with pre-existing cough.
Management
- Stop ACE inhibitor and prescribe angiotensin II inhibitor if needed as an alternative.
- If no improvement, consider alternative diagnosis
Sitagliptin and other dipeptidylpeptidase-4 inhibitors
- A drug sensitivity reaction causing symptoms of cough with rhinorrhoea, dyspnoea, or fatigue.
Bisphosphonates and Calcium Channel Antagonists
- Can exacerbate pre-existing reflux disease leading to reflux cough.
Prostanoid eye drops such as latanoprost
- Can travel down the lacrimal duct and irritate the pharynx leading to cough.
Chronic refractory cough
- Chronic cough with unexplained aetiology despite full investigation, smoking cessation, iatrogenic causes removed and refractory to all treatment.
Management
- Routine referral to respiratory
- Routine Respiratory referral via SCI Gateway for all patients with suspected chronic refractory cough for consideration of neuromodulator medication and possible clinical trial involvement.
Contact the Respiratory Team
- For any queries or concerns contact the respiratory consultants for advice: nhsh.raigmorerespiratory@nhs.scot
Resources
- Smoking cessation referral and additional patient information - https://www.smokefreehighland.scot.nhs.uk/phone-numbers/
- For Patient information on chest clearing techniques The Respiratory resource hub: https://tam.nhsh.scot/respiratory-resource-hub-for-patients-and-carers/my-symptoms/breathing-and-chest-clearance-techniques/
- Stress urinary incontinence in COPD - https://mylungsmylife.org/topics/group-1/stress-urinary-incontinence-and-copd/stress-urinary-incontinence-and-copd/
- For patients with symptoms of dyspepsia: https://gutscharity.org.uk/wp-content/uploads/2018/08/Guts-UK-Non-ulcer-Dyspepsia-Leaflet.pdf
Methods to reduce coughing
- Breathing through your nose as much as you can, rather than your mouth can help. Try to build it up slowly so you are eventually using your nose all the time (except when talking)
- If you feel a cough coming on swallow hard, relax your shoulders and concentrate on breathing slowly and gently out
- Retraining your breathing pattern. Develop good breathing habits by using your diaphragm, rather than muscles around your shoulders and neck to breathe.
- Using airway clearance techniques to help keep your airways clear.
- Try taking regular sips of water can help to keep your throat moist and reduce irritation. Carrying a water bottle with you can help with this.
- Sucking on a sweet can have a similar effect. This can be useful before talking on the phone/ for a long period of time.
- Some people find eating frozen pineapple chunks or frozen grapes can help with cough.
Stop Cough Remedy.
- Try not to cough at all, but if a cough feels like it is to come then cough once only, with hand over mouth and with lips closed.
- Swallow once or sip some water
- Keeping lips closed, breathe out gently, pinch your nose closed and take a breath pause of 5 to 10 secs
- Continue to breathe gently with lips closed for about 15 seconds
- Repeat the breath pause 2 to 3 times, resisting the urge to cough
- ERS guidelines on the Diagnosis and Treatment of Chronic Cough in Adults and Children - Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020; 55: 1901136 [https://doi.org/10.1183/ 13993003.01136-2019]. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children - PubMed
- NICE.Diagnosis | Diagnosis | Cough | CKS | NICE. 2021. Accessed December 7, 2021. https://cks.nice.org.uk/topics/cough/diagnosis/diagnosis/
- Scottish Referal Guidelines for Suspected Lung Cancer - Lung Cancer. 2019. Accessed October 31, 2021. http://www.cancerreferral.scot.nhs.uk/lung-cancer/?alttemplate=guideline
- NICE Bronchiectasis Guidelines -Diagnosis | Diagnosis | Bronchiectasis | CKS | NICE. 2021. Accessed December 7, 2021. https://cks.nice.org.uk/topics/bronchiectasis/diagnosis/diagnosis/
- BTS CAP Guidelines: Pneumonia Adults | British Thoracic Society | Better lung health for all. 2015. Accessed December 15, 2021. https://www.brit-thoracic.org.uk/quality-improvement/guidelines/pneumonia-adults/
- Leichester Cough Questionnaire 2001 https://hgs.uhb.nhs.uk/wp-content/uploads/cough_questionnaire.pdf
- Asthma in adults (Guidelines)
- DVLA Guidance for Cough syncope- Neurological disorders: assessing fitness to drive - GOV.UK. 2021. Accessed December 7, 2021. https://www.gov.uk/guidance/neurological-disorders-assessing-fitness-to-drive
- NHSH ENT guidelines: https://tam.nhsh.scot/for-healthcare-professionals/therapeutic-guidelines/
- NHSH Upper GI guideline: https://tam.nhsh.scot/for-healthcare-professionals/therapeutic-guidelines/gastro-intestinal/upper-gastro-intestinal/upper-gi-guidelines/
- NHSH: Female urinary incontinence (Guidelines)
For any queries or concerns contact the respiratory consultants for advice: nhsh.raigmorerespiratory@nhs.scot
- Smoking cessation referal and additional patient information - https://www.smokefreehighland.scot.nhs.uk/
- For Patient information on respiratory conditions, symptom management, self-management and additional support signpost to: The Respiratory Resource hub- bit.ly/RRH-home
- For Patient and Carer support with their condition, self management and additional support Chest Heart Stroke Scotland: https://www.chss.org.uk/
- For Patient and Carer support with self-management and additional support Lets Get On With It Together: http://www.lgowit.org/
- For patients with symptoms of dyspepsia: https://gutscharity.org.uk/wp-content/uploads/2018/08/Guts-UK-Non-ulcer-Dyspepsia-Leaflet.pdf (Link to be called non-ulcer dyspepsia patient information leaflet.
- Stress urinary incontinence in COPD - https://mylungsmylife.org/topics/group-1/stress-urinary-incontinence-and-copd/stress-urinary-incontinence-and-copd/
| Abbreviation | Meaning |
| ACE | angiotensin-converting enzyme |
| COPD | chronic Obstructive Pulmonary Disease |
| CXR | chest xray |
| ENT | ear nose throat |
| GI | gastroenterology |
| ICS | inhaled corticosteroids |
| ILD | interstitial lung disease |
| NHSH | NHS Highland |
| PE | pulmonary embolism |
| USC | urgent suspected cancer |
- University of Collage London Hospital, Respiratory Physiotherapy Chronic cough leaflet.
- Morice AH, Millqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020; 55: 1901136 [https://doi.org/10.1183/ 13993003.01136-2019].
- NICE.Diagnosis | Diagnosis | Cough | CKS | NICE. 2021. Accessed December 7, 2021. https://cks.nice.org.uk/topics/cough/diagnosis/diagnosis/
- NICE.Diagnosis | Diagnosis | Bronchiectasis | CKS |
-
Lung Cancer. 2019. Accessed October 31, 2021. http://www.cancerreferral.scot.nhs.uk/lung-cancer/?alttemplate=guideline
-
Pneumonia Adults | British Thoracic Society | Better lung health for all. 2015. Accessed December 15, 2021. https://www.brit-thoracic.org.uk/quality-improvement/guidelines/pneumonia-adults/