Diabetes in adults in palliative care (Guidelines)

Pre-terminal disease will influence glycaemic control
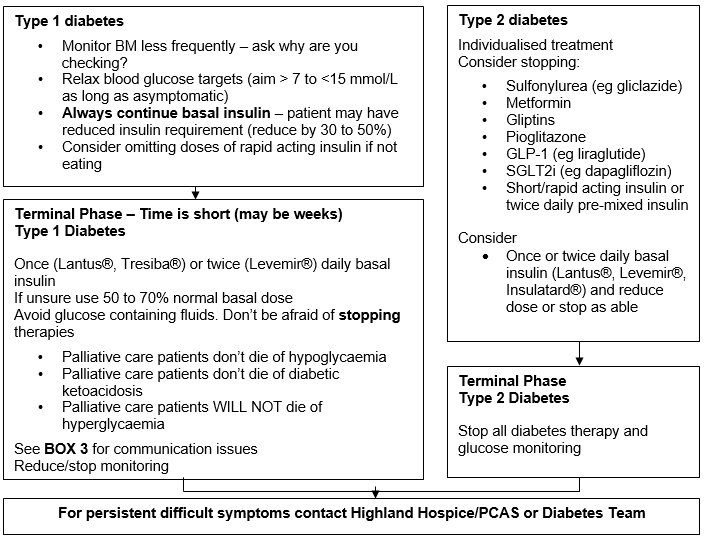
- goal of treatment is to avoid hypoglycaemia and manage symptoms of hyperglycaemia (balance against burdens of additional treatment and monitoring)
- Type 1 diabetes has an absolute insulin requirement (wish to avoid diabetic ketoacidosis)
- little evidence to guide best practice
- individualised treatments, particularly in Type 2 diabetes.
Additional symptom burden to patients may include:
- Hyperglycaemia: dry mouth, thirst, lethargy, blurred vision, polyuria, recurrent infections
- Hypoglycaemia: sweating, hunger, trembling, blurred vision, headache, confusion and disorientation, drowsiness, unconsciousness/coma, seizures.
Potentially reversible issues: infection
- stop or limit drugs which adversely influence blood glucose
- avoid hyperosmotic hyperglycaemic states.
- Anorexia and cachexia
- inability to take food or medicines
- increased hypoglycaemia risk
- Infection
- Metastatic disease
- increased risk of hypoglycaemia (liver, adrenals)
- increased risk of lactic acidosis
- Cirrhosis
- hypoglycaemia risk
- Tumour products
- most promote insulin resistance
- may induce hypoglycaemia
- Cardiac failure
- catecholamine excess leads to insulin resistance
- Renal failure
- Increased risk of hypoglycaemia, and need for reduction in insulin doses
- Pancreatic cancer
- pancreatic destruction may lead to Type 1 diabetes-like insulin deficiency
- Nutritional status
- supplements or nasogastric feeding cause hyperglycaemia
- octreotide:
- inhibits insulin secretion, causing hyperglycaemia
- steroids (given in the morning can cause late afternoon and evening hyperglycaemia)
- orexigenic (stimulates appetite), may contribute to hyperglycaemia
- induce insulin resistance, causing hyperglycaemia.
(Insulin doses are often increased to accompany steroid therapy. If steroids are withdrawn patients are at risk of hypoglycaemia if insulin is not altered quickly or marked hyperglycaemia if all treatment including insulin is stopped and there are still steroids in the system)
- Some diuretics
- Some atypical antipsychotics may increase insulin resistance and cause hyperglycaemia
Patients/families who have lived with diabetes over a long period of time may find a more relaxed attitude to diet and monitoring difficult to come to terms with. It is important that the addition of insulin therapy is not seen as adding to anxiety or withdrawal perceived as abandonment of care.
Individualise monitoring based on patient factors, therapy and goals of care.
| Abbreviation | Meaning |
| BM | Blood glucose |
| GLP-1 | Glucagon-like peptide-1 |
| PCAS | Palliative Care Advisory Service |
| SGLT2i | Sodium Glucose Transporter 2 inhibitor |
Warren, R.E.,Deary, I. J. and Frier, B.M. The Symptoms of Hyperglycaemia in people with Insulin-treated Diabetes:classification Using Principle Components Analysis. Diab Metab Res 2003;19:408-14
Quinn K, Hudson P and Dunning T. Diabetes Management in Patients Receiving Palliative Care. Journal of Pain and Symptom Management. 2006;32(3): 275 -286
Ford-Dunn S, Smith A & Quin J. management of Diabetes During the Last Days of Life: Attitudes of Consultant Diabetologists and Consultant Palliative Physicians in the UK. Palliative Medicine 2006;. 20(:3):197-203
Steven Miller, Clinical Lecturer in Medicine, University of Glasgow, Consultant Endocrinology & Diabetes, and General (Internal) Medicine, Hairmyres Hospital - personal communication to Scottish Palliative Care Pharmacist’s Association Conference 3/9/10.
For Health Care Professionals: End of Life Guidance for Diabetes Care. 2021. https://diabetes-resources-production.s3.eu-west-1.amazonaws.com/resources-s3/public/2021-11/EoL_TREND_FINAL2_0.pdf