Opioid dependence must be diagnosed prior to starting treatment. A comprehensive assessment should be undertaken and include drug screening which is positive for opioid drugs. Drug screens should be interpreted alongside clinical information and should not be treated as definitive themselves.
Patients must be assessed on an individual basis by a health care professional with sufficient knowledge in the use of buprenorphine products to determine suitability of treatment. The patient’s medical history and other prescribed medicines should be considered for contraindications, cautions and interactions when determining if treatment is suitable (see sections: 'Precautions for buprenorphine containing products' and 'Adverse effects').
Baseline liver function testing (LFTs) and documentation of viral hepatitis status is recommended in the Summary of Medicines Product Characteristics (see resources) of all buprenorphine products before starting treatment, however there is little evidence of buprenorphine being likely to cause deranged liver function or liver damage (excepting patients with viral Hepatitis). Baseline LFTs should be taken if clinically indicated. Even when LFTs are indicated, the absence of baseline LFTs should not prevent same day prescribing. Providing there are no immediate and significant clinical concerns regarding liver function, LFTs can be arranged for a later date. (Opioid Drugs in Patients With Liver Disease: A Systematic Review - PMC nih.gov) (see resources).
Patients who have active viral hepatitis infection may be prescribed medicines which interact with buprenorphine, or have existing liver impairment and are at risk of accelerated liver injury. Regular monitoring of liver function is recommended in these patients.
Lower initial doses and careful dose titration in patients with mild to moderate hepatic impairment are recommended. Buprenorphine products are contraindicated in patients with severe hepatic impairment.
Both methadone and buprenorphine can accumulate in patients with hepatic impairment. Clinicians should weigh up the risk of continued illicit drug use versus the risks associated with the prescribed drug and monitor accordingly.
Precipitated withdrawal may occur when buprenorphine is first administered (see section 'Precipitated withdrawal'). If it happens, it typically begins within 1 to 3 hours after the first buprenorphine dose and peaks within 3 to 6 hours before improving. This should be discussed with all patients prior to commencing treatment with buprenorphine products and they should be reassured that, should they experience precipitated withdrawal, symptoms will improve.
Initial Dosing Schedules
To minimise the risk of precipitated withdrawal, and get the maximum benefit from buprenorphine, the patient should be displaying mild signs of opioid withdrawal before administering the first dose of buprenorphine (see Table 1). Use of a clinical opioid withdrawal scale can provide objective and subjective measures for assessing symptoms of withdrawal (see resources).
During titration, daily supervision is recommended (see section 'Supervised self administration of medication') to ensure proper placement of the product in the mouth and to observe patient response to treatment.
Clinicians should contact the community pharmacy to confirm they have stock or allow time to order it in. They should discuss initial dosing instructions and ask them to check that the patient is displaying mild symptoms of opioid withdrawal before they give the first self-administered dose.
If the clinician is not able to assess the patient in person prior to giving the first dose on day 1:
- There should be a clear plan agreed between the clinician and community pharmacist as to how the assessment of opioid withdrawal symptoms will take. The clinical opioid withdrawal scale can be used to measure this (see resources).
- This could be a phone consultation between clinician and patient. Pharmacy staff would then confirm this with the patient in person.
- Another option is to prescribe day 1 doses as a take away dose for the patient to take when they are in withdrawal. This may support same day prescribing where it is clinically appropriate. Supervised administration can then begin on day 2. This is possible due to the relative safety of buprenorphine. Patient understanding of this plan, and how to take the product, must be confirmed.
To reduce the severity and duration of precipitated withdrawal (should it occur) it is recommended that the dose for day 1 is split. Following treatment induction on day 1, the patient should be stabilised to a maintenance dose during the next few days by adjusting the dose according to the clinical effect of the individual patient (Table 2).
Table 1: Induction from full opioid agonists
|
Type of full agonist
|
Current dose of full agonist
|
Point of induction
|
|
Heroin
|
Any dose, any route of administration.
|
When objective and clear signs of withdrawal appear (at least 6 hours from the last use of heroin).
|
|
Methadone
|
Reduce to 30mg daily or lower prior to transfer. Higher doses may lead to precipitated withdrawal or treatment failure where the opioid effect experienced is not enough to cover withdrawal symptoms from cessation of full agonist opioids.
|
When objective and clear signs of withdrawal appear (at least 24 hours from the last use of methadone).
|
|
Opioid Analgesics
|
Any dose, any route of administration
|
When objective and clear signs of withdrawal appear (time will depend on choice of opioid used).
|
Table 2: Dosing during induction
|
|
Buprenorphine and buprenorphine plus naloxone sublingual tablets or film
|
Espranor® Oral Lyophilisate
|
|
Day 1
|
2 to 4mg of buprenorphine followed later in the day by a further 4mg based on individual need.
Maximum dose on Day 1 = 8mg in divided doses.
|
2mg of buprenorphine followed by a further 2 to 4mg later in the day based on individual need.
Maximum dose on Day 1 = 6mg in divided doses.
|
|
Day 2 on
|
The dose can be titrated up to a maximum of 16mg daily on day 2. From day 2 doses should be prescribed as a single daily dose.
Titrate dose in steps of 2 to 8mg buprenorphine guided by assessment of the clinical and psychological status of the patient until the effective maintenance dose is achieved.
|
The dose can be titrated up to a maximum of 12mg daily on day 2. From day 2 doses should be prescribed as a single daily dose.
Titrate dose in steps of 2 to 6mg buprenorphine guided by assessment of the clinical and psychological status of the patient until the effective maintenance dose is achieved.
|
Table 3: Maximum daily doses
|
|
Buprenorphine and buprenorphine plus naloxone sublingual tablets or film
|
Espranor® Oral Lyophilisate
|
|
Maximum Daily Doses
|
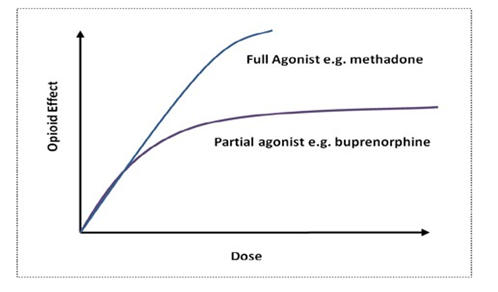
Doses above 16mg are less commonly needed due to ceiling effect. First step is to check placement of tablet / film is correct as this can affect absorption.
Maximum daily doses:
- Buprenorphine plus naloxone products = 24mg/6mg
- Buprenorphine sublingual tablets = 32mg
|
Titrate to a maximum dose of 18mg daily according to patient need.
|
Note: Higher doses of buprenorphine are associated with improved retention in treatment
Less than daily dosing
Less than daily dosing is not commonly used in practice but may be of benefit to some patients, particularly in the later stages of dose reductions. If prescribing in this way, the dose given on any one day should not exceed the product’s licensed maximum daily dose.
Transferring patients between sublingual buprenorphine products and Espranor®
The bioavailability of Espranor® oral lyophilisate (wafer) is higher than sublingual tablets. It has potential to result in an increase in adverse effects (transfer TO Espranor) or symptoms of withdrawal (transfer TO a sublingual product) at the same dose. The following table can be used as a guide to equivalence. Dose can be adjusted according to response which may vary between patients.
Table 4: Suggested Espranor® conversions
|
Buprenorphine Sublingual products (with or without naloxone) dose
|
Approximate equivalent Espranor® dose
|
|
24 to 32mg
|
16 to 18mg
|
|
20 to 24mg
|
16 to 18mg
|
|
10 to 18mg
|
8 to 16mg
|
|
2 to 8mg
|
2 to 8mg
|