History of substance misuse
At the time of admission a full drug and alcohol history should be taken. Clarify what other substances are being taken such as benzodiazepines, cocaine or gabapentinoids and what dose is being taken.
If alcohol dependence is suspected as well as opioid use, the detoxification from alcohol should take precedence. Benzodiazepines prescribed in alcohol detoxification will help some of the symptoms associated with opioid withdrawal.
Opioid withdrawal is uncomfortable but not life threatening, overprescribed opioid replacement is.
Every opportunity should be taken to provide patients with information on harm reduction eg naltrexone and other services and supports available within their area.
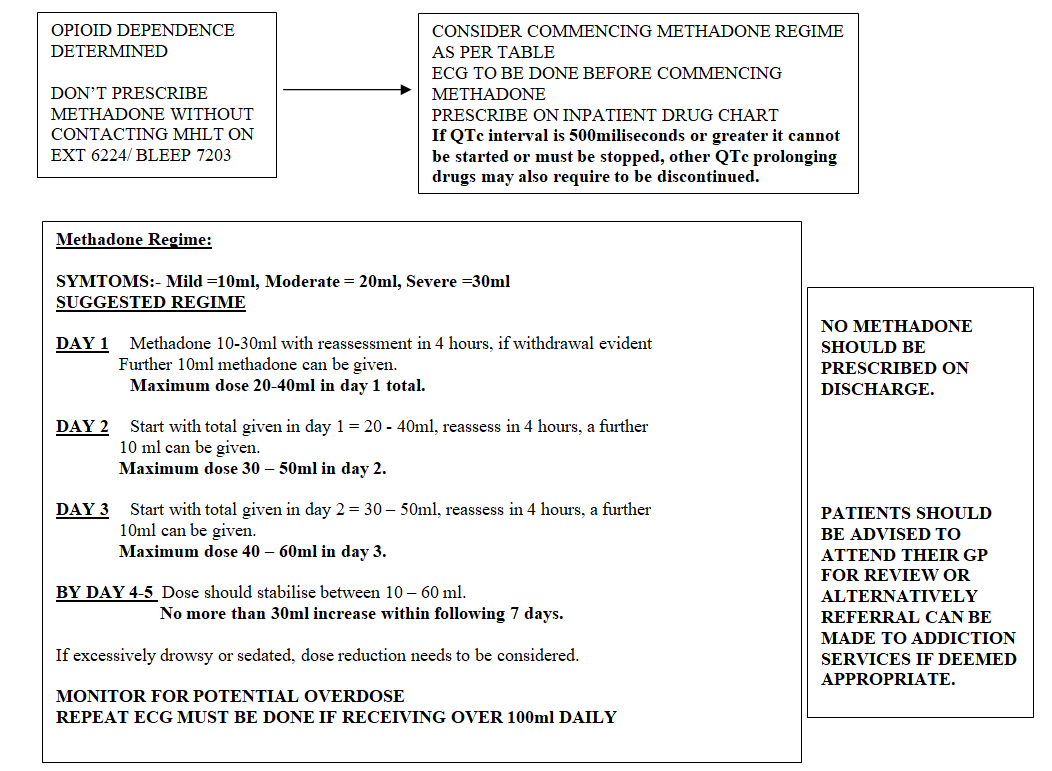
Contact Mental Health Liaison Team on ext 6224 if advice is required.
Establishing past and present contact with services will provide opportunities to confirm history of use.
In line with present guidance all patients should be asked about dependent children/ children in the household establishing –
- names,
- ages,
- is parental drug or alcohol use impacting on them,
- do they require extra support with the children,
- are agencies already involved.
This needs to be handled particularly sensitively to support patients in being as open as possible.
Examination
Examination helps towards confirming history. All injection sites require to be examined and carefully documented. Identifying information regarding complications of drug use and of any current or previous injecting – including localised infections, abscesses, DVTs or damage to peripheral circulation or heart valves, as well as HIV, hepatitis B infection and vaccination, and hepatitis C status. It should also be noted if patients are smelling of alcohol, appear sedated or in withdrawal. (As per orange drug misuse and dependence guidelines 2017)
Signs of opioid withdrawal require to be carefully documented, see opioid withdrawal chart, Appendix 1 at end of document.
If a patients presentation is causing concern (aggressive, agitated, over sedated) do not assume this is caused by their drug misuse. A full examination is required to exclude potential medical causes.
Investigation
Investigation depends on presentation and should be used to verify history and examination.
Blood alcohol levels – establish on admission by use of breathalyser and/or blood ethanol levels to ensure any alcohol problems are identified and treated if necessary.
Patients using drugs may at times find it difficult to provide an accurate history of their drug use, particularly if that results in impairment of consciousness or cognition.
On site instant urine screening for opiates can be particularly helpful in establishing:-
- a baseline of use
- confirming present drug use
- or identifying drugs not declared in a patients history
but they have their limitations e.g. if a patient is prescribed and regularly taking co-codamol or other prescribed opioid medication an opioid test would be positive and therefore it could not confirm whether that individual is taking heroin.