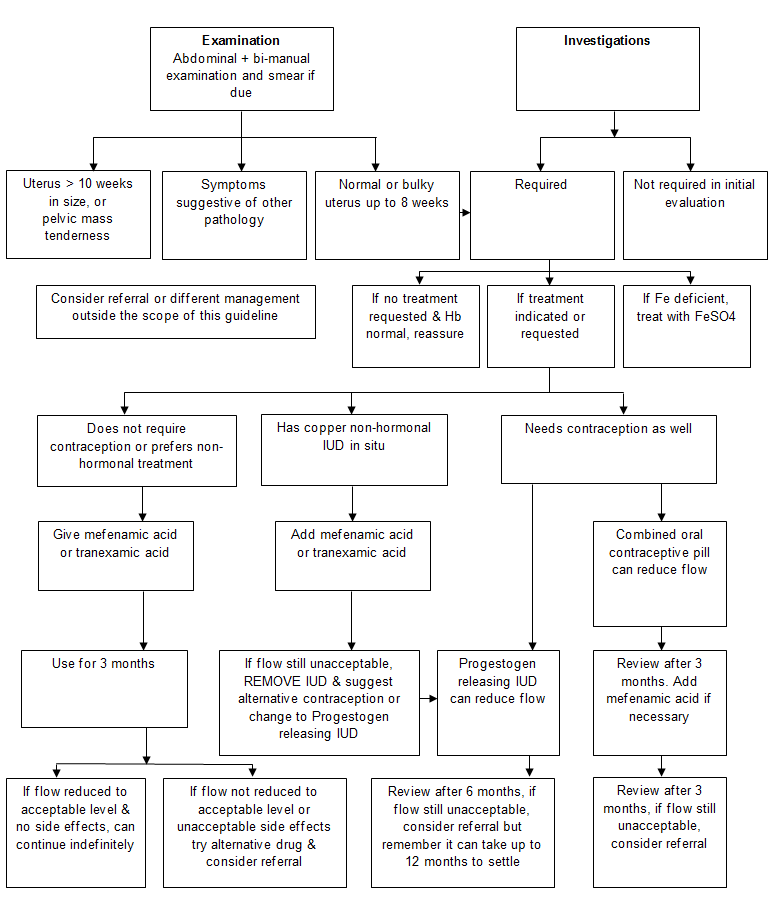
A history of heavy cyclical menstrual blood loss over several consecutive cycles without any intermenstrual or post coital bleeding, should be obtained.
Menorrhagia (Guidelines)

Royal College of Obstetricians and Gynaecologists
History
Examination: Uterus > 10 weeks in size, or pelvic mass tenderness
Refer for ultrasound scan & if pelvic mass check CA125 (immunology brown tube)
Examination: Symptoms suggestive of other pathology
1. Symptoms suggestive of other pathology
-
Irregular bleeding
- Sudden change in blood loss
- Intermenstrual bleeding
- Post-coital bleeding
- Dyspareunia
- Pelvic Pain
- Pre-menstrual pain
2. Risk factors for endometrial cancer
- Tamoxifen
- Unopposed oestrogen treatments
- Polycystic ovary syndrome
- Obesity
Investigations: Required
Add full blood count to initial examination
Investigations: Not required in initial evaluation
No need:
- To arrange a scan if exam is normal;
- To measure ferritin levels;
- For thyroid function tests unless signs and symptoms of thyroid disease;
- No other endocrine investigations are necessary in investigating menorrhagia;
- An endometrial biopsy is not required in the initial assessment.
Mefenamic acid or tranexamic acid given
Mefenamic acid 500mg tds or tranexamic acid 1 g tds starting on first day of period for days of heavy flow
Mefenamic acid or tranexamic acid added
Mefenamic acid 500mg tds or tranexamic acid 1 g tds starting on first day of period for days of heavy flow
Note
Whilst oral luteal phase progesterons are ineffective in reducing menstrual blood loss, intrauterine progesterons are effective
Patient Information Leaflets
Abbreviations
| Abbreviation | Meaning |
| Fe | Iron |
| Hb | Haemoglobin |
| IUD | Intrauterine device |
Editorial Information
Last reviewed: 31/07/2016
Next review date: 31/07/2018
Author(s): Obstetrics and Gynaecology Department .
Version: 2
Approved By: TAM subgroup of the ADTC
Document Id: TAM303