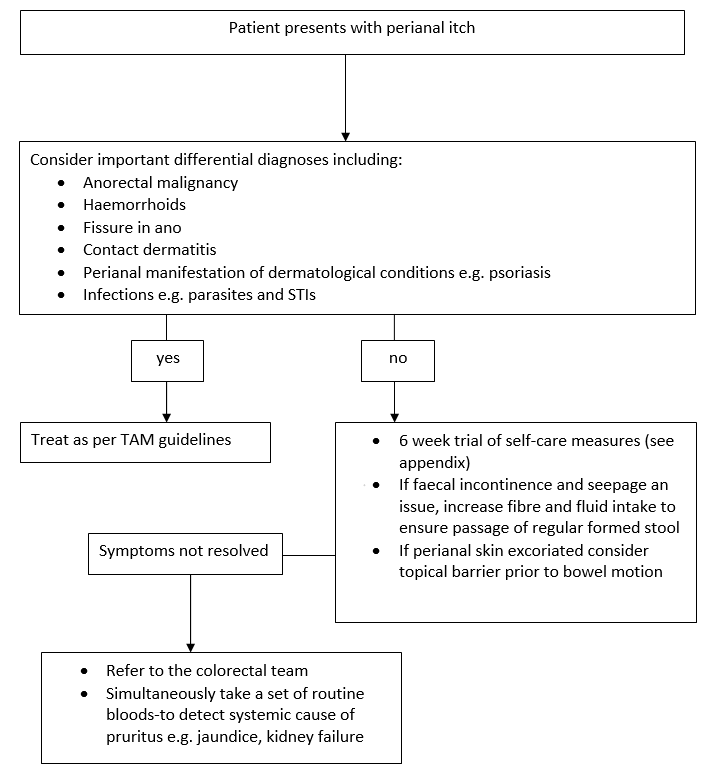
Pruritus ani is generally a diagnosis made after exclusion of several important alternative diagnoses as shown in the flow chart below. Therefore, the history is crucial and some key points on the possible differentials are highlighted below. The treatment options are quite limited, hence the importance of identifying any possible causes that can be eliminated.
- Diet induced diet-induced pruritus is symmetrical, whereas infectious causes lead to an asymmetrical pattern of anal irritation. Avoiding food items known to aggravate pruritus ani these may include coffee, chocolate, citrus fruits, cola drinks, and dairy products. Caffeine is most commonly associated with pruritus. Consider a patient-led symptom diary to record relation to diet.
- Minor faecal incontinence of stool or leakage of mucus secondary to haemorrhoids or rectal prolapse can cause perianal itching and is a common cause of symptoms.
- Perianal infections by fungi (candida), parasites (eg threadworms, pinworms) and sexually transmitted infections can also result in pruritus.
- Primary dermatological conditions such as psoriasis, eczema can affect the perianal to cause itching.