Two key objectives:
- Keep the gluteal fold free of hair that might cause a chronic inflammatory state; keeping the tracts open.
- While there is currently insufficient evidence to make this a general recommendation, multiple laser epilations may result in reduced recurrence of disease. There are several laser clinics in the Highland area offering this service.
- Advise patients that shaving has been associated with disease recurrence.
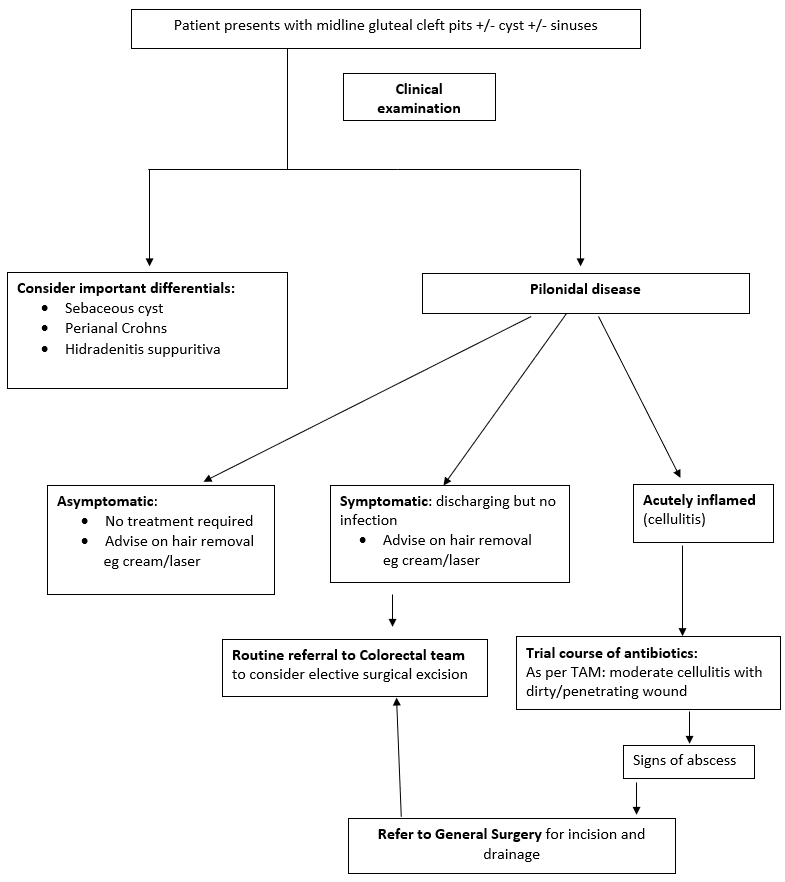
- Triage the patient into one of 4 groups as shown in the flow chart.
- Asymptomatic:
- The patient has the characteristic pits in the gluteal cleft but no discharge or acute inflammation.
- No treatment required at this point.
- Symptomatic (chronic discharge) but no acute inflammation:
- Can be routinely referred to general surgery for elective surgical excision of the affected area.
- Symptomatic (acute inflammation): patient reports pain and redness and swelling, and on examination is tender on palpation, erythema and induration, ie, cellulitis.
- Can be managed with a course of antibiotics with an early review to ensure symptoms settling.
Treat as for Wound infections with minor/moderate cellulitis including facial cellulitis; dirty/ penetrating wound: TAM Cellulitis/Wound Infections (Antimicrobial) | Right Decisions (scot.nhs.uk)
- Can be managed with a course of antibiotics with an early review to ensure symptoms settling.
- Symptomatic (acute inflammation + abscess development):
- Same day referral to General surgery for incision and drainage.
- Asymptomatic: