Adrenarche is the gradual increase in adrenal androgen secretion after approximately the age of 6 years in girls and 7 years in boys. It occurs independently from the gonadotrophin-dependent activation of the gonads in central puberty.
Adrenarche

Purpose of this guideline:
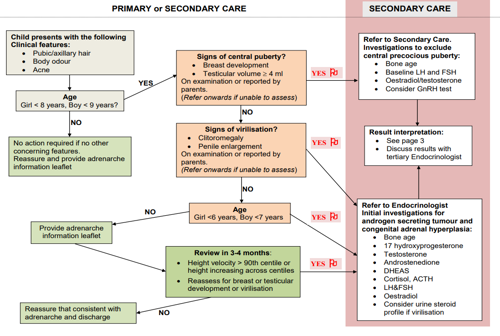
- To guide evaluation of a child presenting with features suggestive of adrenarche.
- To guide the distinction between adrenarche, precocious puberty and other abnormalities of secondary sexual development.
Who should use this guideline:
- general practitioners
- paediatricians
- paediatric endocrinologists.
Patients to whom this guideline applies:
Children presenting with pubic hair growth, axillary hair, body odour and acne before the expected age of puberty.
Adrenarche results in the development of pubic hair, axillary hair, body odour and acne. (It does not result in the enlargement of the breasts, penis or testes).
At the time of adrenarche, there is maturation of the adrenal glands, with increased production of dehydroepiandrosterone sulphate (DHEAS) relative to cortisol. The serum concentration of DHEAS can be used as a marker for the presence of adrenarche, with serum testosterone and androstenedione levels being near the upper limit of the normal range. However, the diagnosis can be made on clinical features without further investigations.
Adrenarche is a normal variant of pubertal development. It is important to distinguish this from precocious puberty and virilising conditions such as androgen secreting tumours and congenital adrenal hyperplasia. Adrenarche itself does not require treatment*.
*There has been previous concern that adrenarche may be associated with the development of insulin resistance, polycystic ovarian syndrome and metabolic syndrome, but this does not alter management or follow-up.
(Please view this table in landscape mode on mobile devices)
| Breast / testicular development | Clitoral / penile growth | Linear growth acceleration | Bone Age | Androgens | Gonadotrophins | |
| Premature adrenarche | Absent | Absent | Absent, or slight initial acceleration | Up to 2 years advanced on chronological age Correlated with height age | Early pubertal, DHEAS may be moderately elevated | Prepubertal |
| Precocious puberty | Stage 2+ breast development ³ 4ml testicular volume | Absent or early | Progressively accelerated | Progressively accelerated | May be normal or elevated for age Oestradiol may be elevated | Early pubertal (If suppressed consider oestrogen secreting tumour) |
| Congenital adrenal hyperplasia | Absent | Enlargement | Moderately to markedly accelerated | Moderately or markedly advanced for age and pubertal stage | Moderately to markedly elevated | Prepubertal |
| Virilising tumours | Absent | Marked and progressive enlargement | Markedly accelerated | Markedly and progressively advanced | Markedly elevated | Prepubertal or suppressed |
| Iatrogenic | Absent | Marked and progressive enlargement | Markedly accelerated | Markedly and progressively advanced | Markedly elevated testosterone | Prepubertal or suppressed |
- Williams RM, Ward CE, Hughes IA. Premature adrenarche. Arch Dis Child 2011; 97: 250-254.
- Bourguignon JP, Rosenfield RL. Precocious pubarche. Practical Algorithms in Paediatric Endocrinology 2007.
- Ibanez L, Valls C, Marcos MV et al, Insulin sensitization for girls with precocious pubarche and with risk for polycystic ovary syndrome: effects of prepubertal initation and postpubertal discontinuation of metformin treatment. J Clin Endocrinol Metab 2004; 89: 4331-7.
- Ibanez L, Diaz R, Lopez-Bermejo A et al. Clinical spectrum of premature pubarche: links to metabolic syndrome and ovarian hyperandrogenism. Rev Endocr Metab Disord 2009; 10: 63-76.
- Idkowiak J, Lavery GG, Dhir V et al. Premature adrenarche: novel lessons from early androgen excess. Eur J Endocrinol 2011;165:189-207.
- Ghizzoni L, Milani S. The natural history of premature adrenarche. J Paediatr Endocriol Metabol. 2000;13 Suppl 5:1247-51