Key Principles:
- Primary goal is rapid definitive haemorrhage management.
- Inform ODPs and CEPOD theatre team early if patient requires surgical management.
- Excessive blood pressure causes bleeding:
- Target MAP 50-60 mmHg or SBP of 80 - 100mgHg
- Elderly patients/ isolated head injury
- Target MAP 60-70 mmHg or SBP of 110mmHg
- Use volume and calcium to manage blood pressure
- Correct coagulopathy early
- Deliver a balanced transfusion with early use of FFP to manage endotheliopathy.
- DO NOT GIVE CRYSTALLOID before definitive haemorrhage control.
- DO NOT GIVE VASOPRESSORS before definitive haemorrhage control.
- Manage hypocalcaemia (ionised Calcium <1.0mmol/l) and hyperkalaemia proactively
- Note: Calcium chloride can be used if central access is available.
- Maintain normothermia
- Minimise patient movement to prevent clot disruption.
- Communicate physiological parameters regularly with the surgical team.
Prepare
Equipment
- Airway Trolley
- Blood Transfusion Board and blood delivery team
- Belmont Rapid Infuser
- Cell salvage
- Large Volume Central and Peripheral Access
- Underbody Warmer
- ROTEM
- Warm Theatre (25°C)
Monitoring
- Use standard AAGBI monitoring.
- Do not delay haemorrhage control to establish invasive monitoring
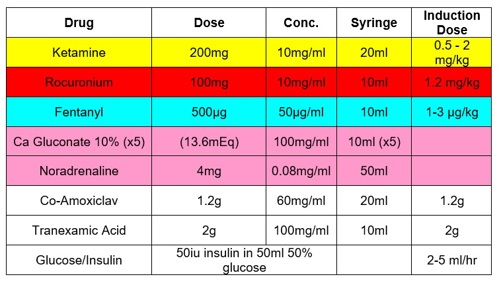
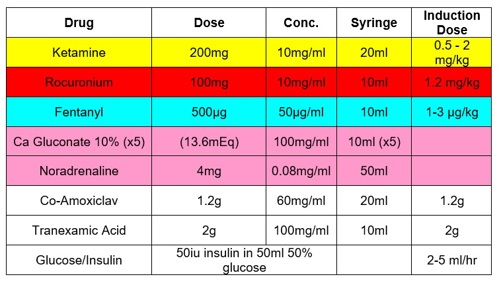
Drugs
Blood Management:
- Declare Code Red
- Highlight an area as a 'blood station' where blood can be received, checked and documentation completed.
- Use 'Bloods Boards' to facilitate balanced transfusion.
- Target an empiric PRC:FFP ratio of 1:1
- Order an initial 'TRAUMA PACK A'
- 4 units universal/type specific PRC and 4 units universal FFP
- Pre-thawed plasma is available and will be delivered to the emergency department. 4 units of FFP will be automatically thawed by BTS when these units are dispatched.
- Proactively order a 'Pack B' if high transfusion requirement.
- 6 units PRC, 6 units FFP, 1 pool platelets, 2 units cryocpreiptate.
- Anticipate transfusion requirements
- Adult, male code red patients may receive RhD O Positive Red Cells.
- Early ROTEM
- Use ROTEM to supplement balanced transfusion.
- See document ‘Management of Trauma Induced Coagulopathy’
- Ensure blood is available and checked prior to induction.
- Do not give cryoprecipitate unless evidence of hypofibrinogenaemia
Tranexamic Acid (TXA)
The following adults should receive 1g TXA*:
- at risk of bleeding
- confirmed bleeding and a HR >110 and/or SBP <90mmHg or
- GCS <13 with evidence of head injury.
Give a further 1g bolus if there is:
- bleeding requiring ongoing resuscitation and/or hemorrhage control.
- Confirmed intracranial hemorrhage in patients with GCS <13
- Hyperfibrinolysis or viscoelastic studies
The maximum total dose is 2g. Where all criteria are met it may be appropriate to administer a 2g bolus.
*Do not give first dose of TXA >3hours from injury unless evidence of hyperfibrinolysis.
Induction & Maintenance of Anaesthesia:
- Ensure surgeons are scrubbed and ready
- Prepare and drape patient
- Pre-oxygenate
- Consider OPA + 2 x NPA to optimise
- Certain circumstances may require a more tailored or delayed approach to allow safe induction (e.g. to optimise oxygenation or cardiovascular status)
- Manual In-Line Cervical Spine Care
- Consider Reverse Trendelenburg position
- Anticipate Hypotension on Induction
- Ensure Rapid Infuser connected, functional and loaded with blood and products.
- Reduce drug doses and volatile concentration
- (aim 0.3-0.5 MAC until haemodynamically adequate)
- Antibiotics
- Aim to deliver 300-500mg fentanyl slowly over first half an hour following definitive haemorrhage control.
Communication
- Ensure optimal team communication until definitive haemorrhage control.
- Discuss Damage Control Vs Definitive Surgical options with operating team
- Insert a stop point at 15min intervals (when clinically appropriate) using the following structure ‘SCOTCH”:
- Surgical Progress
- Damage Control Vs Definitive Surgery
- Coagulation and Transfusion Management
- What blood and blood products have been administered?
- What is in the room?
- What is on order?
- ROTEM analysis
- Oxygen Debt/Acidaemia
- Lactate/Base Excess Trend
- Temperature
- Calcium and Electrolytes
- Ionised Calcium and replacement given
- K+
- Heading
- Time since commencement of surgeon
- Anticipated duration
- Do we need any further assistance?
- Post-operative plan
- Further imagine?
- Critical Care?
Post Definitive Haemorrhage Control
- Aim to restore normal physiology
- Use base deficit and lactate to guide volume resuscitation
- ROTEM may be used to deliver targeted coagulopathy management
- Consider Noradrenaline, if required, only once circulating volume is restored and definitive haemorrhage control achieved.