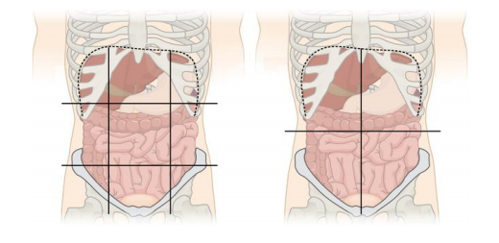
Abdominal quadrant regions by Jmarchn is licensed under CC BY-SA 3.0
Blunt abdominal trauma presents a greater diagnostic challenge than penetrating trauma, where operative indications are usually more obvious. All abdominal trauma is managed via one of three pathways
- Operative management
- Non-operative management (NOM) with IR
- NOM without IR
Key Clinical Principles
- Suspect rather than rely on numbers - abdominal haemorrhage is often concealed, is always non compressible and recognition is challenging.
- The surgical hand will only detect 50% of intra-abdominal injuries, even in conscious patients
- Be extra cautious with elderly, obese, obtunded and spinal cord-injured patients
- Abdominal injuries may extend above the costal margin- trauma does not respect anatomical zones.
- Do not remove the pelvic binder to perform a laparotomy
- Patients with a sustained SBP <70mmHg and abdominal trauma should probably be in theatre.
- Ureteral injuries are rare but commonly missed
Surgery
- A midline laparotomy is the preferred approach.
- Aim for Haemorrhage control within 1 hour of hospital arrival.
- A consultant surgeon should be present for all trauma laparotomies.
- Common indications for immediate trauma laparotomy:
- Haemodynamically unstable with positive FAST
- Peritonitis
- Unstable patient with free fluid on CT
- Hollow viscus injury
- Retained weapon
- Gunshot wound
- Evisceration
- Free fluid on CT without solid organ injury (consider strongly)
Damage c=Control Surgery (DCS)
- Utilise damage control principles (proximal control, haemostasis and faecal/urinary diversion) over definitive procedures in selected patients with physiological compromise.
- Temporary abdominal closure should be considerd in unstable patients..
- Plan at second-look laparatomy at 24-72 hours.
Imaging
CT
- CT is the gold standard for blunt abdominal trauma
FAST
- Useful in unstable patients or mass casualty triage.
- Positive FAST can rule-in intra-abdominal haemorrhage, but a negative FAST does not rule it out.
Ultrasound
- Ultrasound should not be used acutely to assess intra-abdominal injury in adults. CT is modality of choice.



