This procedure involves the removal of a specified amount of blood by venepuncture, every 3 to 4 weeks and as tolerated, to control iron overload. Venesections should continue, if well tolerated, until ferritin reaches values < 300 microg/L or the liver iron concentration is <5mg/g dry weight.
Prior to each venesection procedure the following should be done, as a baseline:
- Weight, baseline temperature, pulse, respirations and blood pressure;
- Ensure patient is well clinically and that there are no active clinical issues of concern;
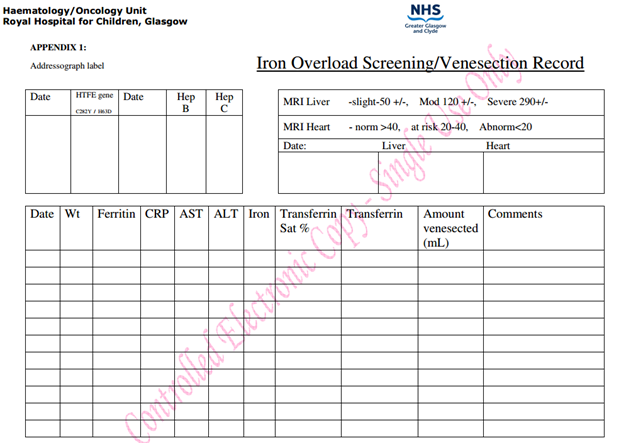
- Send FBC, reticulocytes, U&Es, LFT’s, serum iron, transferrin, transferrin saturation, ferritin, CRP and document these in the iron overload screening chart (see Appendix 1)
Ensure that the patient is fully informed of the procedure and any questions are answered.
If there is a history of fainting - lie flat for procedure and 30 minutes after completion.
The nurse must always ensure that the patient is feeling well and that he/she has eaten as hunger/dehydration can lead to fainting during or post procedure.
The patient’s blood count must be checked prior to carrying out procedure and results from last venesection (e.g. ferritin and iron levels).
The amount of blood to be venesected must be calculated prior to each venesection based on the patient's weight (5-7mls/kg to max 350mls) or previous amount venesected/comments on chart (e.g. fainted after 200mls taken)
Patient is cannulated and venesected over 30 mins or slower.
First blood specimen removed is used for laboratory tests.
Patient should be allowed to sit up after procedure and have a sugary drink (parents are asked to bring a sweet drink at each visit). If required 5-10ml/kg of normal saline can be administered.
After 15-30 minutes patient may be discharged if well.
Precautions explained to child/parent prior to each discharge:
- Keep activity to a minimum on same day (e.g. no active sports) especially if returning to school
- If feeling faint (cold, clammy) within few hours after venesection:
- sit down and put head between knees or lie flat
- have a sweet drink if possible
- stay sitting/lying until feeling better
- slowly get back onto feet
- Take it easy for rest of day.
- Inform ANP or DCU of fainting episode or unwell after discharge.