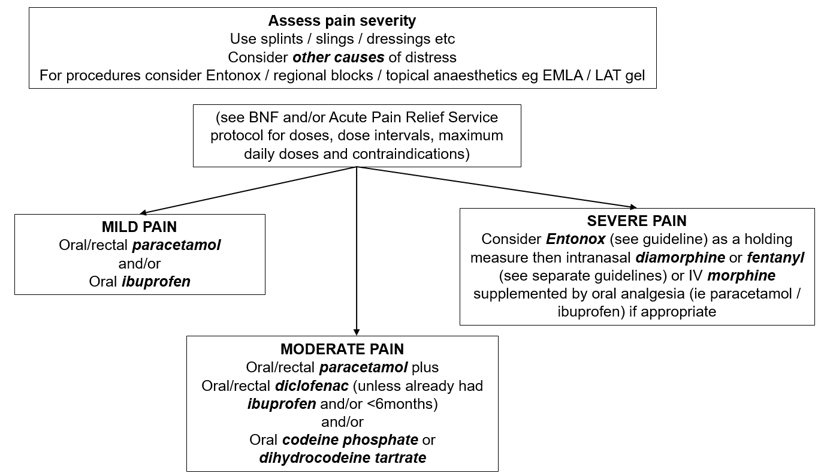
Pain in children can be difficult to assess (for example the child may not appear distressed or have difficulty describing / admitting to pain). This can lead to pain being under-recognised, under-treated and treatment being delayed. Drug choice and dosage may also cause problems in those not used to treating children due to unfamiliarity.
Pain management in children, paediatric emergency medicine (335)

What's new / Latest updates
24/10/2025 Pain algorithm updated and diamorphine guideline added
Objectives
- Recognise pain in children and provide analgesia for moderate & severe pain within 20 minutes of arrival in the Emergency Department
- In treating pain, attention should be paid to other factors distressing the child such as fear of unfamiliar environment and people, parental distress, people in uniforms, needle avoidance, fear of injury severity etc.
Scope
Patients presenting to the Paediatric Emergency Department.
Audience
Medical and nursing staff in the Paediatric Emergency Department.
- Pain assessment should be repeated frequently to ensure adequate response to any intervention.
- In the Emergency Department of the Royal Hospital for Sick Children, it is the experience of the Triage Nurse that is used to gauge the severity of a child’s pain, based on their observation and feedback from parents.
For example:
| No Pain | Mild Pain | Moderate Pain | Severe Pain | |
| Behaviour | Normal activity No↓ in movement Happy |
Rubbing affected area Decreased movement Neutral expression Able to talk/play normally |
Protective of affected area ↓movement / quiet Complaining of pain Consolable crying Grimaces when affected part moved / touched |
No movement or defensive of affected part Looking frightened Very quiet Restless, unsettled Complaining of lots of pain Inconsolable crying |
| Injury example* | Abrasion / small laceration Ankle sprain Minor head injury |
Small burn / scald Undisplaced limb # Fingertip injury Appendicitis |
Displaced limb # # dislocation Larger burns/scalds Appendicitis Sickle crisis |
* Example of injury is only intended as a guide – cases should be assessed on an individual basis
If child is being admitted and is likely to need ongoing analgesia for moderate / severe pain, consider contacting pain relief nurse specialist (ext. 84320), Pain Team (ext 84319) or duty anaesthetic registrar (page 18602).
- Psychological strategies: involving parents, cuddles, child-friendly environment, and explanation with reassurance all help build trust. Also, distraction with toys, blowing bubbles, reading, portable DVD players or story-telling can help to alleviate pain.
- Non-pharmacological adjuncts such as limb immobilisation for fractures and dressings for burns.
Prescribe diamorphine via intranasal route (in mg) based on child’s weight (see chart – round to nearest weight; final dose=0.1mg/kg) and use chart to determine the volume of water to add to a 5mg diamorphine ampoule. Mix well.
- Draw up 0.2 mls (0.1mg/kg) of the resultant solution into a 1ml syringe and discard the rest (following controlled drugs procedure)
- Attach atomiser (MAD device WolfeTory®) to the 1ml syringe.
- Position patient either sitting up at 45° or with head to one side
- Administer dose by inserting into nostril loosely and aim for centre of nasal cavity prior to squirting
- Depress the plunger in a steady quick single motion.
- Hold atomiser in place for further 5 seconds to prevent medication from dribbling out of nostril
- Intranasal diamorphine is usually effective within 5-10 minutes but allow up to 20 minutes for maximal pain control
- Continue 02 sats monitoring for 1 hour post administration. Analgesic effect lasts up to 4 hours.
Guidelines for making up Intranasal Diamorphine Solution
- dilute 5mg of diamorphine powder with specific volume of sterile water
|
Weight (kg) |
Volume of sterile water to be added |
Final dose in mg (in 0.2mls) |
|
10 |
1ml |
1mg |
|
11 |
0.9ml |
1.11mg |
|
12 |
0.85ml |
1.18mg |
|
14 |
0.7ml |
1.43mg |
|
16 |
0.6ml |
1.67mg |
|
18 |
0.55ml |
1.82mg |
|
20 |
0.5ml |
2mg |
|
25 |
0.4ml |
2.5mg |
|
30 |
0.35ml |
2.86mg |
|
35 |
0.3ml |
3.33mg |
|
40 |
0.25ml |
4mg |
|
≥50 |
0.2ml |
5mg |
- to be used in conjunction with Emergency Department Pain Management guideline
Indications:
To be included as part of the first-line treatment of severe pain in a child (without IV access).
For example, in children with pain secondary to:
- Clinically suspected limb fractures
- Painful/distressing burns
Contraindications:
- Need for immediate IV access (use parenteral morphine)
- Significant nasal trauma
- Blocked nose or upper respiratory tract infection
- Age < 1 year (or weight < 10kg)
- General contraindications/sensitivity to fentanyl or other opioid use
- Significant head injury
- MAOI anti-depressant within 14 days
Adverse Effects:
- Adverse effects are uncommon, but may include:
- Respiratory depression
- Hypotension
- Nausea and vomiting
- Itch
- Chest wall rigidity (only reported in rapid large IV doses)
Protocol:
- Weigh the child in kg, attach monitor for continuous O2 saturations
- Draw up calculated dose of Fentanyl according to weight
- Attach atomiser (MAD device WolfeTory ®) to the 1ml syringe (if total calculated dose over 1ml then draw up additional dose volume in another 1ml syringe)
- Position patient either sitting up at 45° or with head to one side
- Administer dose by inserting into nostril loosely and aim for centre of nasal cavity prior to squirting
- If the dose is > 0.6mL, split dose between both nostrils to prevent loss of solution by sneezing or swallowing.
- Depress the plunger quickly
- Hold atomiser in place for further 5 seconds to prevent medication from dribbling out of nostril
- Don’t forget to give supplementary oral analgesia (if not contra-indicated) and that the child may need ongoing IV analgesia once the initial pain is controlled
- Continue 02 sats monitoring for at least 1 hour post administration
- Therapeutic levels are reached within 2 minutes and may last for up to 30 minutes. The dose can be repeated after 30 minutes if adequate analgesia is not achieved after the first dose.
Intranasal FENTANYL guideline for dosing and administration
Dose = approximately 1.5 micrograms/kg (repeat after 30mins if needed)
Preparation: Fentanyl injection 50 micrograms in 1ml (CD) (dilution not required)
|
Weight of child (kg) |
Dose (micrograms) |
Dose volume (to 1 decimal place) |
|
10 |
15 |
0.3 ml |
|
13 |
20 |
0.4 ml |
|
15 |
25 |
0.5 ml |
|
20 |
30 |
0.6 ml |
|
25 |
40 |
0.8 ml |
|
30 |
45 |
0.9 ml |
|
35 |
55 |
1.1 ml |
|
40 |
60 |
1.2 ml |
|
45 |
70 |
1.4 ml |
|
50 |
75 |
1.5 ml |
|
55 |
85 |
1.7 ml |
|
60 |
90 |
1.8 ml |
Approved by RHC ED Consultant group with approval from RHC Drugs and Therapeutics Committee pending: February 2022