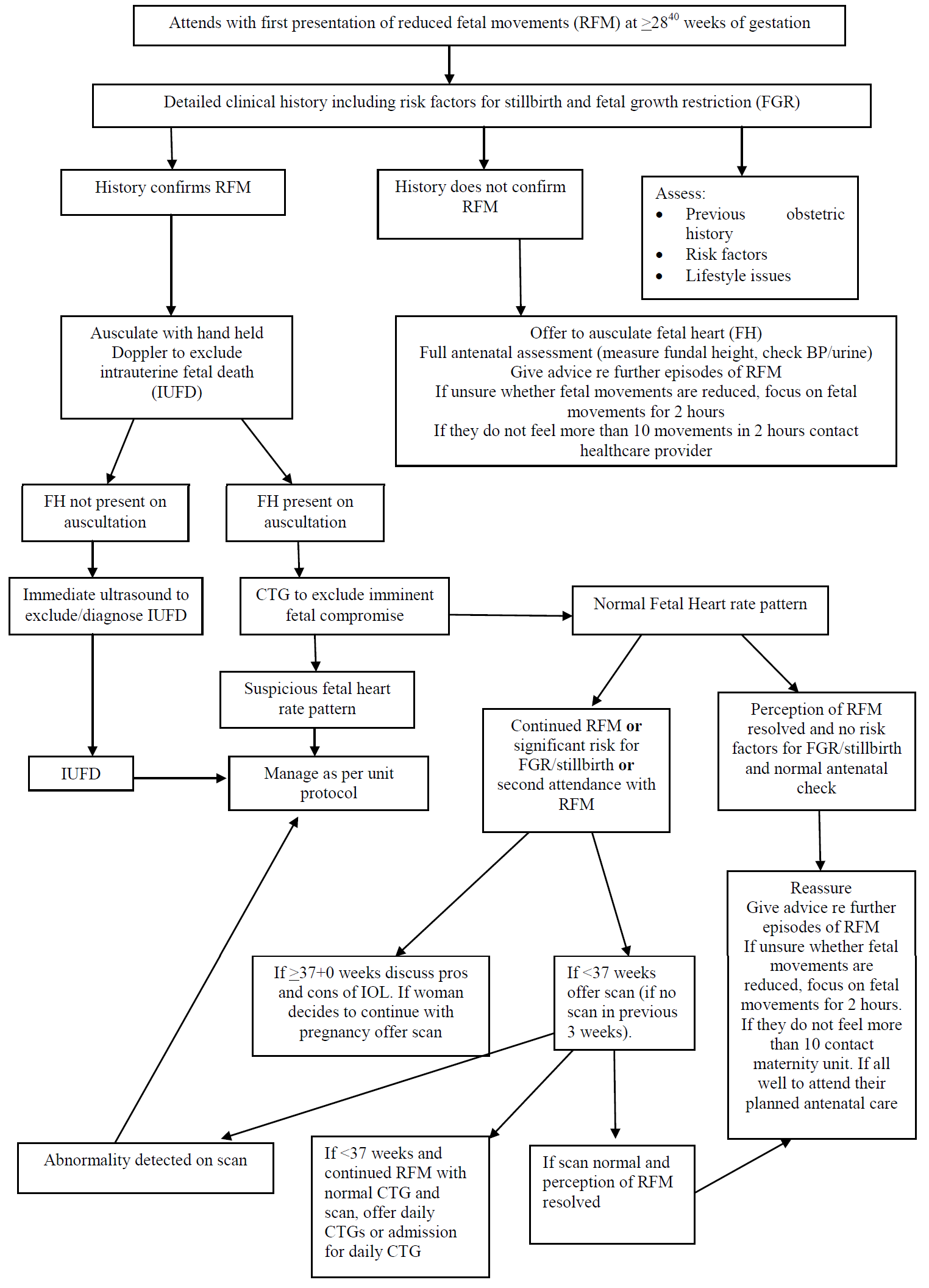
Women who have normal clinical assessment and investigations after second (or more) episode of RFM should undergo a scan (including umbilical artery Doppler) for fetal well being (unless they have had a normal scan within 3 weeks). At the third presentation, the woman should be referred to the consultant-led antenatal clinic for consideration of increased fetal surveillance.
Those women who are still not feeling fetal movements after having a normal scan and CTG should be offered either daily CTGs as an outpatient or admission and twice daily CTGs until movements return.
Women who present on two or more occasions with RFM are at increased risk of a poor perinatal outcome. There are no studies to determine whether intervention (e.g. delivery or further investigation) alters perinatal morbidity or mortality. The decision whether or not to induce labour at term in a woman who presents recurrently with RFM when the growth, liquor volume and CTG appear normal must be made after careful consultantled counselling of the pros and cons of induction on an individualized basis (RCOG Green Top Guideline No. 57)



 Reduced fetal movements at ≥ 28+0 weeks assessment form (pdf)
Reduced fetal movements at ≥ 28+0 weeks assessment form (pdf)