Intermittent claudication is characterized by pain in the muscles of the leg brought on by exercise and relieved by rest. It is usually caused by atherosclerosis which causes narrowing or occlusion of the arteries supplying these muscles. Most commonly the muscles of the calf are affected as the commonest site for atherosclerosis in the leg is in the superficial femoral artery. Patients walk for a certain distance and then complain of a severe cramping pain in the calf muscles. They rest for a few minutes, the muscle recovers and they can walk a similar distance again. The muscles of the thigh and buttock can also be affected if the atherosclerosis is more proximal, affecting the aorta or iliac arteries.
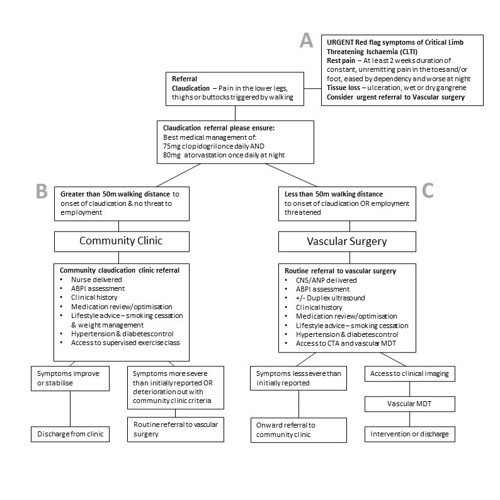
In general, intermittent claudication is a benign condition, with 75% of patients either remaining the same or improving, and most never deteriorate to a level where the viability of the leg is at risk. Only 5 – 10% of claudicants will find that their symptoms deteriorate such that they develop Chronic Limb Threatening Ischaemia (CLTI). This is characterized by constant, unremitting pain at rest (usually in the toes and forefoot, not the muscles of the leg) of at least 2 weeks duration, ulceration and/or gangrene and requires prompt assessment and intervention by a vascular specialist.
Acute limb ischaemia is where the patient suffers sudden onset, catastrophic ischaemia characterized by a pale, perishing cold paralysed, paraesthetic, pulseless limb, often caused by embolic disease. This is a vascular emergency and patients need immediate referral to a vascular specialist.
As intermittent claudication poses no limb threat in the significant majority of patients, the risk of intervention usually outweighs the benefit, and so most claudicants should be treated conservatively. In addition, if lifestyle changes are implemented, the claudication distance usually improves. Such measures include weight loss, regular exercise and smoking cessation. Whilst claudication usually has a benign course in terms of the affected limb, it is a marker that the patient has atherosclerotic disease, a systemic condition affecting all vascular beds. As such they are at increased risk of cardiovascular events such as myocardial infarction and stroke and should have cardiovascular risk factors such as hypertension and diabetes addressed and be started on an antiplatelet agent and a statin.

 Scan the code to visit our website
Scan the code to visit our website