Introduction to Deep Brain Stimulation (DBS) for Tremor or Dystonia
You have been referred or are considering Deep Brain Stimulation (DBS) as a treatment for Tremor or Dystonia. The information here has been written to give you further information on this. You can also get further information from the team.
In the following sections we use the term “tremor” to include conditions such as Essential Tremor and Dystonic Tremor although we may also consider people with other types of tremor for DBS. We use the term “dystonia” to include various types of dystonia, which may be generalised or more limited to a particular group of muscles.
What is Deep Brain Stimulation?
We can use Deep Brain Stimulation as a treatment for some people with Tremor or Dystonia. ![]()
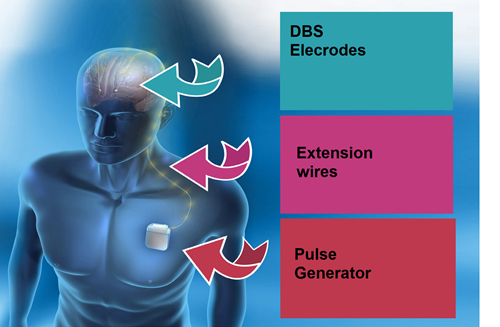
This involves very fine wires with electrodes at their tips being implanted into the brain. The electrodes send a continuous electrical pulse through them to change some of the electrical signals in the brain and reduce the symptoms of tremor or dystonia.
These wires are connected to extensions that are tunnelled under the skin behind the ear and down the neck. They are connected to a pulse generator (a device like a pacemaker) that is placed under the skin usually in the chest area.
Modern hardware is now much smaller than it was in the past and it is unusual for patients to be bothered by this. The team can show you examples of what the kit looks like.
You will either be asleep (general anaesthetic) for the whole process, or have sedation which means you will be awake but relaxed during part of it. Your consultants will discuss this with you and your preferences will be accommodated where possible.
The team in Glasgow’s Queen Elizabeth University Hospital have been implanting stimulators since 2004, and run the national DBS service for the whole of Scotland.
Images courtesy of Medtronic and Abbott




