Click here for printable versions of this leaflet in:
| English | Arabic عربى | Mandarin普通话 |
| Polish (Polskie) | Romanian (Română) | Urdu اردو |


This advice is intended for parents/carers taking their child home after consulting a doctor. Your doctor may recommend different treatments depending on your child's condition.
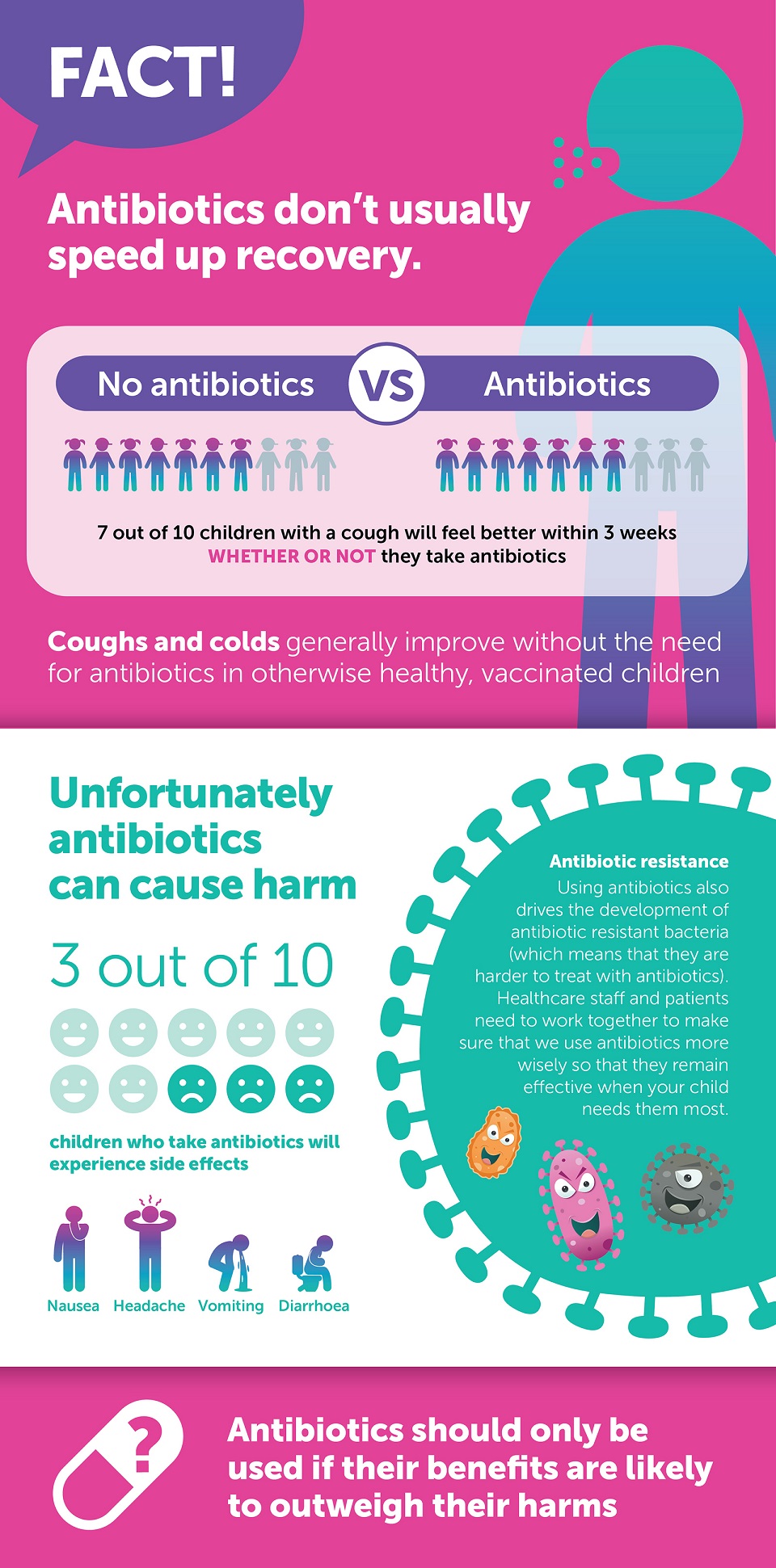
Most children with coughs/colds do notneed treatment with antibiotics. Antibiotics do not treat viral infections. They usually will not help your child get better more quickly. They often cause side effects such as rash and diarrhoea. They will also promote the development of antibiotic resistant bacteria in your child.
Antibiotics are usually only considered if your child has a high fever for more than 24 hours and is breathing faster than normal plus using extra effort when breathing. If your child has a wheeze and difficulty breathing, they are unlikely to benefit from antibiotics but may benefit from inhalers.
In addition, if your child has any amber or red features above, they will need to be urgently seen by a healthcare professional who may decide that your child may benefit from additional treatment.
You can help relieve symptoms by:
It can take a few weeks for a child to fully recover from a cough. Children rarely cough up phlegm, but they are still clearing their chest. If you are worried that after an initial improvement, their cough getting significantly worse, or not getting better after 4 weeks, you should take your child to see their GP. Most children make a full recovery from a chest infection with no lasting effects
It is not always easy to stop your child catching these infections. Good hygiene practices can reduce the spread of viral infections:
Use the table below to help you know what to do if your child is unwell.
 |
|
|---|---|
|
If your child has any of the following:
|
You need help now: Go to the nearest Hospital Emergency Department or phone 999 |
 |
|
|---|---|
|
If your child has any of the following: If your child has any of the following:
|
You need to see a doctor or nurse today. Please ring your GP surgery or call NHS 111 - dial 111 |
 |
|
|---|---|
|
If your child has none of the red or amber features |
Self care You can keep looking after your child at home. If you are still concerned about your child, call NHS 111 – dial 111 |
Content adapted with permission from the what0-18.nhs.uk resource produced by the Healthier Together initiative

We are one of the leading paediatric care centres in the UK, and the largest in Scotland. We provide family centred care to newborns, infants, children and young people both in hospital and in the community.
https://www.glasgowchildrenshospitalcharity.org/