Situation: how long should therapeutic Direct Oral Anticoagulants (DOACS) be discontinued prior to elective surgery?
Background
- DOACS are widely used for therapeutic anticoagulation; indications include non-valvular atrial fibrillation thromboprophylaxis, thromboprophylaxis post arthroplasty and treatment of arterial/venous thromboembolism.
- Advantages include fixed patient dosing and lack of requirement for therapeutic monitoring.
- Without a routine therapeutic monitoring test, guidance is required as to when to discontinue DOACS prior to surgery.
Assessment: DOACs include factor Xa Inhibitors (rivaroxaban, apixiban, edoxaban) and direct thrombin inhibitors (dabigatran)
Factor Xa Inhibitors:
These produce competitive reversible antagonist of activated factor X (Xa). Factor Xa catalyses the conversion of prothrombin to thrombin.
Dosing1:
| |
Prophylaxis DVT/PE |
Treatment DVT/PE |
Non valvular AF |
| Rivaroxaban |
10mg od |
15mg bd 3 weeks
20mg od (maintenance)
|
20mg od |
| Edoxaban |
|
30mg od (≤61 kg)
60mg od (>61kg)
|
30mg od (≤61 kg)
60mg od (>61kg)
|
| Apixiban |
2.5mg bd |
10mg bd |
5mg bd |
Pharmacokinetics1:
| |
Rivaroxaban |
Apixiban |
Edoxaban |
| Half-life(h) |
5-13 |
8-15 |
10-14 |
| Renal elimination % |
66 |
27 |
50 |
| Time to maximal action (h) |
1-4 |
1-4 |
1-2 |
As illustrated above renal function effects the efficacy of factor Xa inhibitors.
Rivaroxaban – manufacturer advises caution/dose reduction if CrCl 15-30 ml/min and avoidance if CrCl below 15ml/min.
Apixiban - manufacturer advises caution/dose reduction if CrCl 15-30 ml/min and avoidance if CrCl below 15ml/min.
Edoxaban - manufacturer advises caution/dose reduction if CrCl 15-30 ml/min and avoidance if CrCl below 15ml/min.
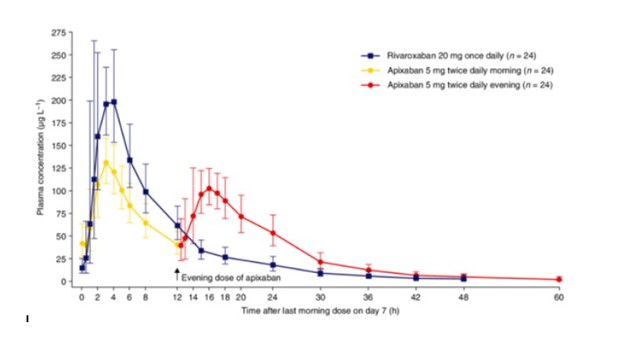
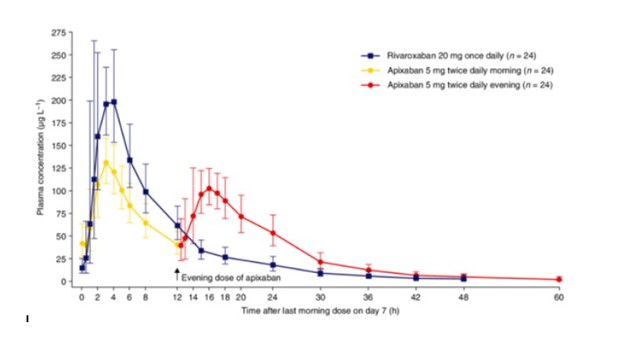
The half-life of rivaroxaban and apixaban (with normal renal function) are demonstrated by their concentration-time graphs2:
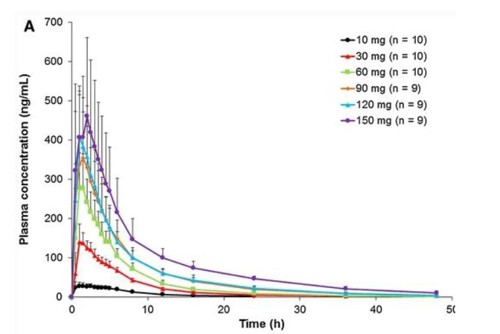
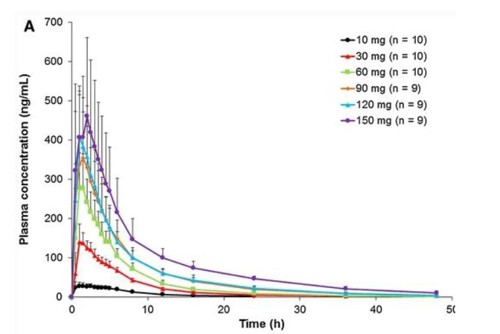
The half-life of edoxaban is demonstrated by the following concentration-time graph [Usual dose 30mg od (≤61 kg) and 60mg od (>61kg)]3:
Perioperative considerations:
From the half-life data and concentration-time graphs, it is apparent that with normal renal function, by 24 hrs post dose (~ 2 half-lives) the plasma concentration and therefore clinical anticoagulation is significantly lower than peak levels.
Surgery/anaesthetic procedures can be classified as either low risk/consequence of bleeding or high risk/consequence of bleeding.
Low risk surgery/procedures would include those where direct pressure can stop bleeding with low risk of harm e.g. body surface surgery or fascia iliaca block. High risk surgery would include: major body cavity surgery, vascular surgery, and spinal/neurosurgery. High risk anaesthetic procedures would include central neuraxial blockade.
For low-risk procedures, omission of a single dose and proceeding 24 hours post dose is acceptable. For high-risk procedures, 48 hours should elapse4.
For ease of management/to allow regional anaesthesia, elective patients should therefore be advised to take their last dose of rivaroxaban, apixiban or edoxaban 48 hours preoperatively.
When restarting therapeutic dosing, maximal anticoagulation can be expected 4 hours post dose.
Renal impairment:
Where patients have CrCl below 15-30 ml/min, accumulation / greater anticoagulation may be seen; this is more likely with rivaroxaban/edoxaban than apixiban. In this situation, omission longer than 48 hours may be needed.
Emergency Surgery:
Where patients require emergency surgery, for most FVRH specialties e.g. general surgical laparotomy or major trauma surgery, it is likely that by 24 hours post dose the risk of bleeding is manageable. Within 24 hours of dosing, where there is a significant risk of surgical bleeding, haematology advice should be sought.
Regional Anaesthesia:
18-24 hours should elapse post dose prior to removing an epidural catheter (dosing not recommended with catheter in situ) and dosing should not restart within 6 hours of removal.
Ideally, 48 hours should elapse post treatment dose before conducting epidural or spinal anaesthesia.
AAGBI guidelines on management of hip fracture patients indicate that 24 hours post dose, spinal anaesthesia.
AAGBI guidelines on management of hip fracture patients indicate that 24 hours post dose, spinal anaesthesia, anaesthes(with normal renal function) may be considered depending on individual patient risk assessment5.
Monitoring:
Routine monitoring of Rivaroxaban, Edoxaban or Apixiban is not performed; Prothrombin time is extended but should not be used for monitoring or making management decisions.
Reversal:
In most circumstances, specific reversal will not be needed, but within 24 hours of dosing/active bleeding this can be considered.
Andexanet alfa is a modified recombinant inactive form of human factor Xa that binds to and blocks the effects of factor Xa inhibitors. It is approved for reversal of apixaban and rivaroxaban in cases of bleeding. However, its use to reverse the effects of edoxaban is currently off-label6.
Where andexanet alfa is not available, alternative agents include prothrombin complex (beriplex/octaplex) and tranexamic acid.
Bridging:
The PAUSE Trial (Perioperative Management of Patients with Atrial Fibrillation Receiving a Direct Oral Anticoagulant) looked at DOAC cessation prior to elective surgery7; for low risk bleeding surgery last dose of DOAC was given 24 hours preop and restarted 24 hours post op; for high risk bleeding surgery last dose was given 48 hours preop (Dabigatrin up to 72 hrs dependent on renal function) and restarted ~ 48 hours post op. Rates of bleeding ranged between 0.9-1.85% and rates of arterial thromboembolism were 0.16-0.6% (90% post op). DVT incidence was 0.1% and PE 0.2%. The study concluded that routine bridging was not needed.
Therefore, unless at particularly high risk of embolism, patients will not be routinely clexane bridged; this is based on the short duration without anticoagulation and the intermediate baseline risk of thromboembolic events.
Where there is a high risk of thromboembolism, the most pragmatic strategy may be omission of a single dose/proceeding with surgery 24 hours post dose, as long as the risk of surgical bleeding is not high.
Where the oral route is unavailable for more than 48 hours post-operatively, individual daily review of the risk of bleeding v thromboembolism is required to determine if post-operative enoxaparin bridging is indicated.
Direct thrombin inhibitor:
- Dabigatran is a prodrug which is hydrolysed to its active from which directly inhibits thrombin (Factor II).
- Dabigatran’s half-life is 12-17 hrs. However, Dabigatran undergoes 85% renal elimination, hence dosing and duration of action is much more dependent on renal function than the Factor Xa inhibitors1.
- Indications include: Prophylaxis post arthroplasty surgery (75-220mg od dependent on patient age, renal function and drug interactions), Treatment of thromboembolism (110-150 mg bd dependent on patient age, renal function and drug interactions) and non valvular AF (110-150mg bd dependent on patient age, renal function and drug interactions).
- Dabigatran is not recommended where CrCl is below 30ml/min and dose reduction is recommended where CrCl is 30-50 ml/min.
Perioperative considerations:
Dabigatran should be omitted for at least 48 hrs prior to elective procedures, but this period should be increased in the presence of renal impairment4:
CrCl > 80ml/min 48 hours
CrCl 50-80ml/min 72 hours
CrCl 30-50ml/min 96 hours
The Summary of Product Characteristics provides a full list of cautions, contraindications and interactions.
When restarting therapeutic dosing, maximal anticoagulation can be expected 2 hours post dose.
Emergency Surgery:
Where surgery is performed within 24 hours of dabigatrin dosing or in the presence of renal failure, Haematology advice should be obtained.
Regional Anaesthesia:
Association of Anaesthetists Guidelines recommend 48-96 hours cessation prior to central neuraxial block depending on renal function; this contrasts with 72-120 hours recommended by the American Society of Regional Anesthesia (ASRA). Dosing is not recommended with an epidural catheter in situ and 6 hours should elapse after catheter removal prior to dosing4.
Monitoring:
Routine monitoring of dabigatrin is not recommended; thrombin time is a marker of dabigatran activity, but is not commercially available. aPTT is also elevated but is not sufficiently sensitive to use as a clinical marker. PT may also be increased.
Reversal:
In most circumstances, specific reversal will not be needed, but within 24-48 hours of dosing/active bleeding this can be considered.
Praxibind (idarucizumab) is a monoclonal antibody licenced to specifically reverse dabigatrin8.
Where idarucizumab is not available, alternative agents include prothrombin complex (beriplex/octaplex) and tranexamic acid.