The following exercises are for the early and later stages of your rehabilitation. It is important to follow the instructions and monitor how you are doing. Load is needed to aid recovery but overload may worsen your pain.
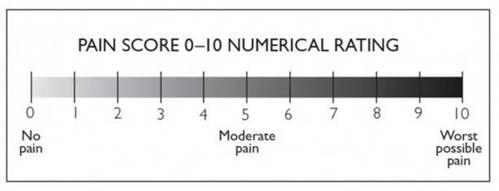
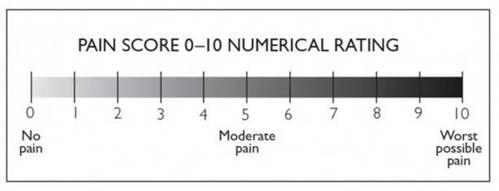
Try to work at a level no higher than 2 on the below scale with the exercises and general physical activity.
1. Exercises for early stages


- Lying on your back on your bed or the floor, with knees bent and feet on the surface. Tighten your buttock muscles, and slowly lift your bottom up, and slowly lower back down.
- Perform 3 sets of 10 repetitions.
- Lying on your back on your bed or floor with straight legs. Tighten your thigh muscles, pushing the backs of your knees down into the bed/ floor.
- Hold for a count of 5 seconds. Relax. Perform 3 sets of 10 repetitions.
When the previous exercise is pain free, move on to this one.

- Sitting in a chair with support at your lower back. Straighten your affected leg out in front, straightening the knee and toes pointing up towards the ceiling. Hold for 5s.
- Perform 3 sets of 10 repetitions.

- Lie on your unaffected side. Make sure your top leg is in line with your body. Lift the leg up towards the ceiling and slowly lower back to the starting position.
- Perform 3 sets of 10 repetitions.
2. Exercises for later stages

- Stand with your back against the wall, with feet hip width apart and away from the wall. Slowly slide down the wall as far as you are comfortable. Then slowly push back up again. Perform 3 sets of 10 repetitions.
- Once this is entirely comfortable, do this without the support of the wall.

- Once the previous exercise is pain-free, try this with one leg. Stand on your affected leg, letting the knee bend as far as comfortable.
- Then place your unaffected leg on the floor, pushing back up straight. Perform 3 sets of 10 repetitions.