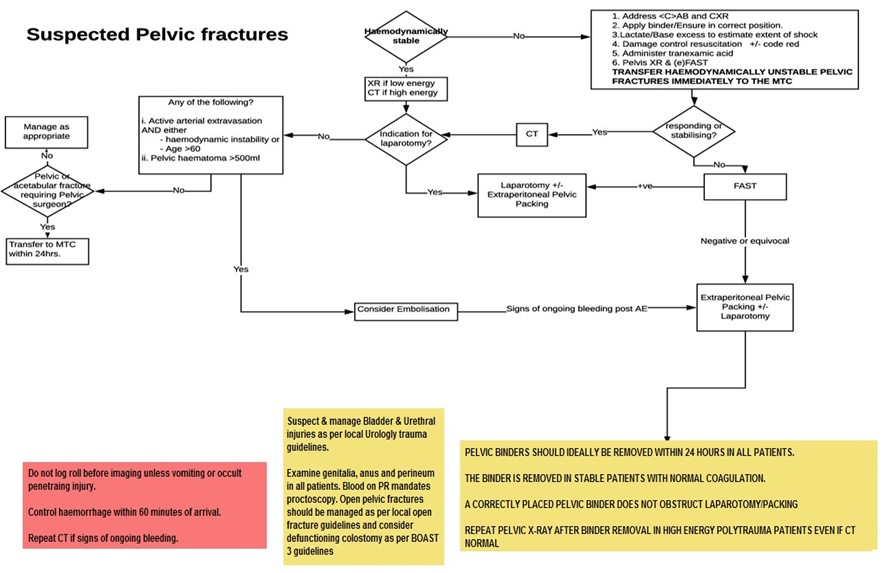
- Is the patient haemodynamically stable?
- Is the pelvic fracture mechanically stable?
- Are there other sites of bleeding including chest and abdomen?
- Is the fracture open? (perineum, rectum, vagina)?



Mortality of up to 35% is reported with pelvic bleeding. Haemorrhage control should be achieved within 60 minutes of the patient’s arrival.
Most haemorrhage (>70%) is venous and can be controlled by:
Transfer to the MTC patients with:
X-ray is Indicated in the following:
eFAST is used in pelvic fracture patients deemed too unstable for CT.
Use CT for suspected high-energy pelvic fractures.


The absence of extravasation does not exclude pelvic haemorrhage. Consider repeating triple phase CT if clinical signs of ongoing bleeding.
Indications:
Relative Indications:
The pelvic binder (or pelvic external fixator) should remain on during laparotomy and EPP. If a laparotomy is required, perform this first.
A pelvic retroperitoneal zone III injury from blunt trauma should not be explored from within the abdomen.
Extra-Peritoneal Packing from a supra-pubic incision is indicated in the following patients:
Pelvic Binders are a resuscitation aid and should be removed once resuscitation is complete in patients who are normothermic with no further bleeding and normal coagulation. This is usually within 24 hours of admission.
Consider external fixation in patients undergoing laparotomy and/or EPP with deranged physiology and those receiving damage control surgery only after discussion with a specialist pelvic surgeon.
Should be performed within 24 hours in stable patients without deranged physiology Patients with deranged physiology should have definitive fixation delayed.
The lower abdomen, groin, buttocks, perineum, anus, rectum, and vagina must be examined in all cases for wounds. This can be performed intra-operatively or after imaging as appropriate.
A positive PR exam for blood mandates a proctoscopy. A positive PV exam for blood mandates a colposcopy.
Debridement should occur:
Wounds to the anus and rectum, and some buttock and perineum wounds often require a defunctioning stoma and general surgery input. The principles of which are: