Requirements/Equipment
Appropriate area
Appropriately designated area for NIV according to site protocol eg A&E, Medical HDU, ITU
Trained member of staff to set up NIV and monitoring
NIV machine (Draeger Savina)
Tubing, facemask, filter, exhalation port
Oxygen supply, suction facilities
SaO2 and ECG monitoring equipment
Acute NIV Patient Care Plan and Prescription chart (available in HDU/For download on Firstport link).
This must be completed by middle grade/senior medical staff prior to commencement. Setting changes, observations and blood gases must be documented on the NIV Monitoring Chart (add appendix).
Initial Set Up
- Select appropriate mask using the sizing tool.
- Ensure exhalation port, filter/water trap, tubing, bacteria filter and oxygen tubing are connected.
- Turn on machine and wait for self-check to finish.
- Ensure oxygen is connected.
- Select settings for Draeger Savina
Mode Spon-CPAP-PS (CPAP with Pressure Support)
Dial PEEP (EPAP)
Dial PS (Pressure support).
PEEP + PS = IPAP
Dial FiO2 to achieve target saturation 88-92%
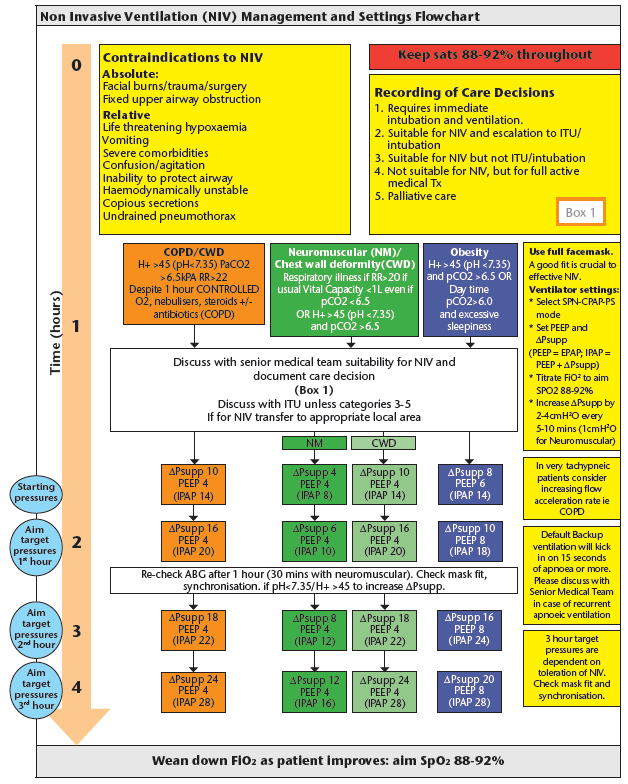
Please refer to NIV Flow Chart for initial starting pressure depending on indications.
- Encourage the patient to breath in and out whilst holding the mask close to face to allow acclimatisation. Once the patient is comfortable, adjust the head gear with straps to ensure minimal leak. Care needs to be taken to ensure the mask is not fitted too tightly to reduce pressure sores.
- Titrate Pressure Support (PS) in 2-4cmH2O increments every 5-10 minutes interval (1cmH2O every 10 minutes for Neuromuscular) as tolerated to achieve good chest/abdominal movement and reduced respiratory rate. Titrate FiO2 to achieve target saturation. Refer to flowchart for titration of pressures depending on indications.
Monitoring
Arterial blood gas (ABG)
Perform ABG 1 hour post initiation of NIV, and at 4-6 hour intervals. ABGs should be done 1 hour after any change in ventilator settings.
Vital signs
Continuous SPO2 monitoring
Monitor RR, HR, BP every 15 mins for first hour then hourly
Check patient comfort, air leak/mask leak and synchronisation.