- HFpEF accounts for approximately 50% of patients with heart failure
- The incidence of HFpEF increases with age. The Female: Male ratio is 2:1.
- Associated conditions include AF, Hypertension, CKD, Diabetes, Obesity, Amyloidosis
- The presentation is the same as for Heart Failure with reduced Ejection Fraction (HFrEF/LVSD)
i.e. breathlessness, fatigue, reduced exercise tolerance, signs of fluid retention (oedema, raised JVP, pulmonary congestion) - Hospitalisation rates, QoL and mortality are all like HFrEF/LVSD
- Most (80%) will have a raised BNP
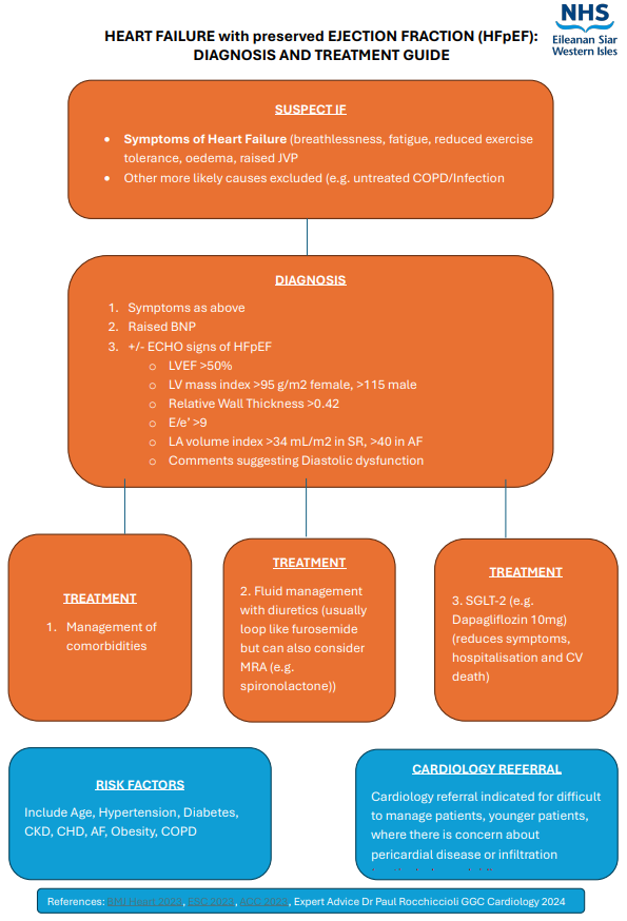
Diagnosis and treatment guide

More patients are receiving a diagnosis of HFpEF from clinic attendance, ECHO or directly in Primary Care. The following is intended a simple guide to diagnosis and management. This is for information only, and it is up to individual clinicians if they feel they have the knowledge and capacity to manage this patient cohort.
- Bloods: BNP, U+E, FBC, TSH, LFT, HbA1C, serum electrophoresis and urine for Bence Jones proteins (some cases are caused by Amyloidosis)
- ECHO will show no signs of HFrEF/LVSD, but the following markers may be commented on suggesting HFpEF
- LV mass index >95g/m2 (female), >115g/m2 (male)
- Relative wall thickness >0.42
- LA volume index >34 ml/m2 (if in Sinus Rhythm),>40ml/m2 (if in AF)
- E:e’ ratio at rest >9
- Signs and Symptoms of Heart Failure
- LVEF >50% on ECHO
- Raised BNP +/- ECHO evidence of structural/functional diastolic dysfunction.
- The Cardiac Nursing service and Rehab service do not see patients with HFpEF
- If help is required a General Medical referral would be appropriate initially. Cardiology referral indicated for difficult to manage patients, younger patients, where there is concern about pericardial disease or infiltration (particularly amyloid).
- The treatment summary is suitable for primary or secondary care
- Loop diuretics (e.g. Furosemide) can relieve symptoms associated with HFpEF (occasionally an MRA (e.g. Spironolactone) may be added for symptoms control)
- SGLT-2 drugs (e.g. Dapagliflozin and Empagliflozin) have been shown to reduce symptoms and improve QoL and reduce a combination of hospitalisation and cardiovascular death and are recommended in HFpEF
- Optimal risk factor and co morbidity management can reduce symptoms in HFpEF