Set changes
We recommend set changes every 3 days, and those using steel cannulas should change every 2 days.
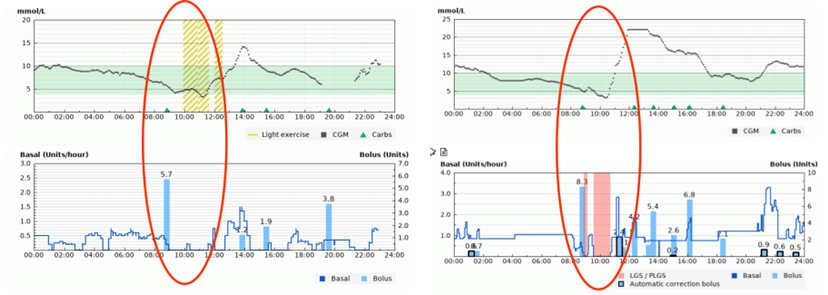
If sets are kept in place for longer than this then the absorption of insulin from the site becomes less effective. This often leads to glucose readings above target.
Remember to rotate your cannula sites. Repeated use of the same sites will lead to problems with insulin delivery.
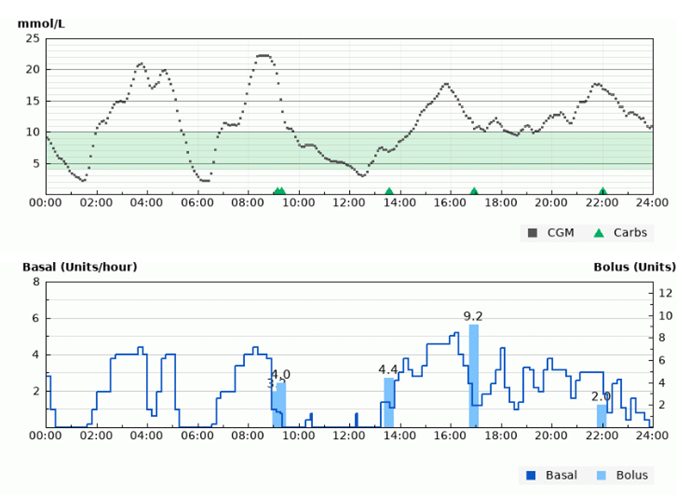
If you are using HCL therapy and your glucose readings are rising above target despite the system delivering more insulin, you should assume the problem is with your infusion set and change it ASAP.
Boluses
Number of boluses per day
When you are using an insulin pump you should aim to bolus for all meals and snacks. Being on HCL does not replace the need to bolus. We therefore expect most children and young people to bolus at least 5 times per day. Generally, we do not expect those on HCL to do extra manual boluses for corrections, unless something unusual has happened like a set failure.
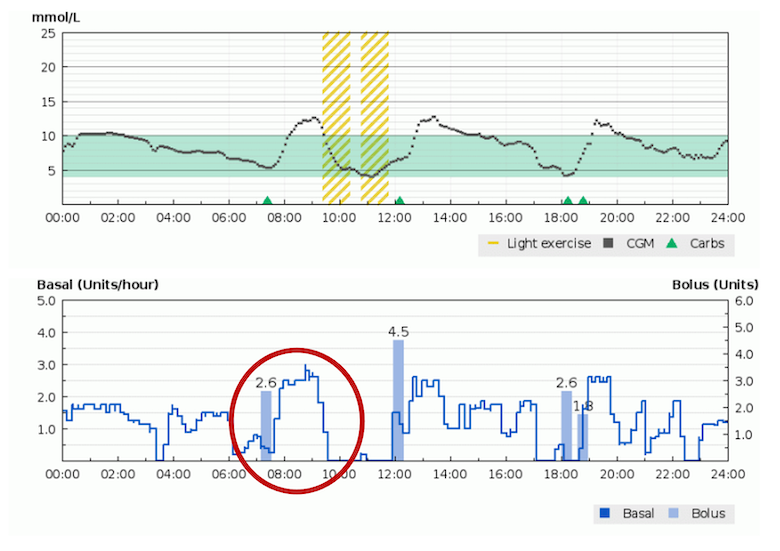
Timing of boluses
Even rapid acting insulin, such as novorapid, still takes time to be absorbed from the subcutaneous tissues. In order for boluses to be most effective they should be delivered before eating. This is arguably even more important for those on HCL as discussed further below (see bottom section).
Average carbohydrate intake per day
In order to be confident that you are remembering to bolus for all of your meals and snacks, you can look at your average carbs per day entered through your pump. The table below broadly lists what we would expect children of different ages to consume, although of course everyone is slightly different.
| Average grams of carbohydrate per day | ||
| Age | Female | Male |
| 1-3 years | 115g | 125g |
| 4-6 years | 170g | 185g |
| 7-9 years | 205g | 220g |
| 10-12 years | 255g | 270g |
| 13-14 years | 285g | 315g |
| 15-16 years | 300g | 360g |
| 17-18 years | 310g | 390g |
Time spent in automode
“Automode” is when your pump and sensor are communicating with each other and your insulin is being adjusted automatically. If this stops working, your pump will revert to “manual mode” and the pre-programmed settings. Reasons for this could include:
- loss of connectivity between pump and sensor
- failure to calibrate your sensor with a fingerprick blood glucose check when asked.
You should aim to spend more than 90% of your time in automode. If this is not the case, then it is more difficult to draw conclusions from your HCL data.