Parent information leaflet to download
What is prolonged Jaundice?
Jaundice is described as a yellowing of the skin, and sometimes of the whites of the eyes. It occurs in 90% of newborn infants. Prolonged jaundice is the term for jaundice which is still present after 2 weeks in term babies (>37 wk) and 3 weeks in preterm babies.
What causes prolonged jaundice?
Jaundice is caused by a buildup of bilirubin, a dark yellow substance. This is a natural waste product of the normal breakdown of red blood cells. Before birth, the mother’s liver removes the product, but after birth the baby’s liver must get rid of it on its own.
However, the liver is still immature in newborns, so it is less efficient at clearing waste products. These can build up in the skin and appear as jaundice.
Jaundice usually appears after 2-3 days and gradually disappears on its own by 14 days. However jaundice can often last longer, especially in the breastfed or preterm baby.
Does prolonged jaundice matter?
Prolonged jaundice is usually related to breast milk feeding and is harmless. In this case, jaundice will disappear in the coming weeks and you should continue breastfeeding your baby.
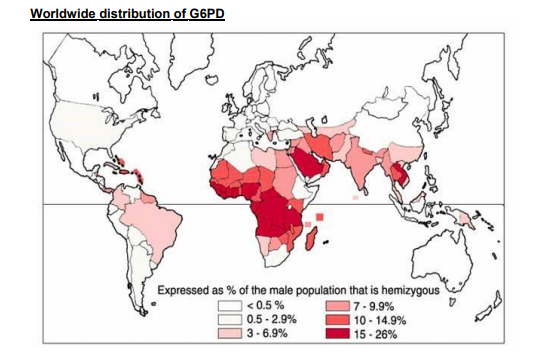
Very rarely prolonged jaundice can be a sign of liver, thyroid, metabolic or blood problem. This is very uncommon but must be investigated so that treatment can be given if required.
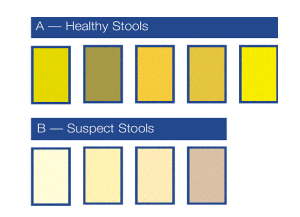
If your baby develops dark urine, pale stools or is not thriving seek advice from health visitor or GP
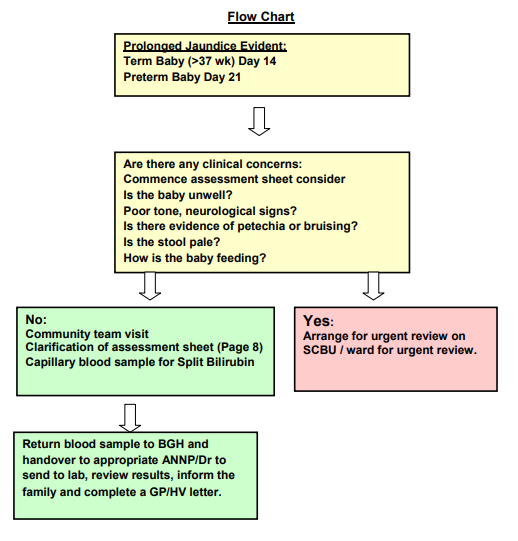
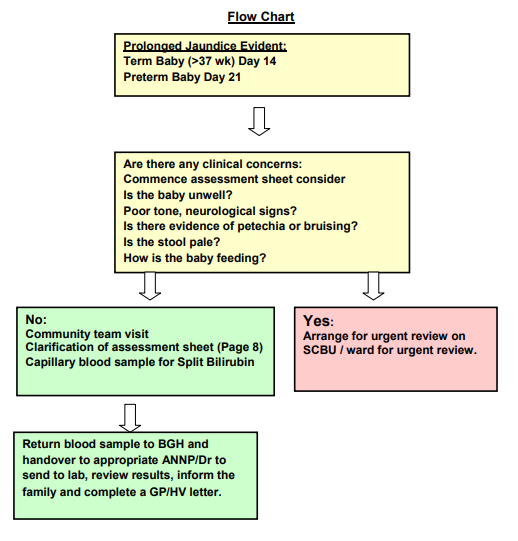
What to expect if your baby remains jaundice?
Term babies who remain jaundice at 15 days and preterm babies who remain jaundice at 22 days will be referred to the children’s dept at the BGH to be reviewed by a member of the neonatal team within the following week.
If prior to this appointment there are any clinical concerns an urgent referral for review should be
made via HV/GP/NHS 24.