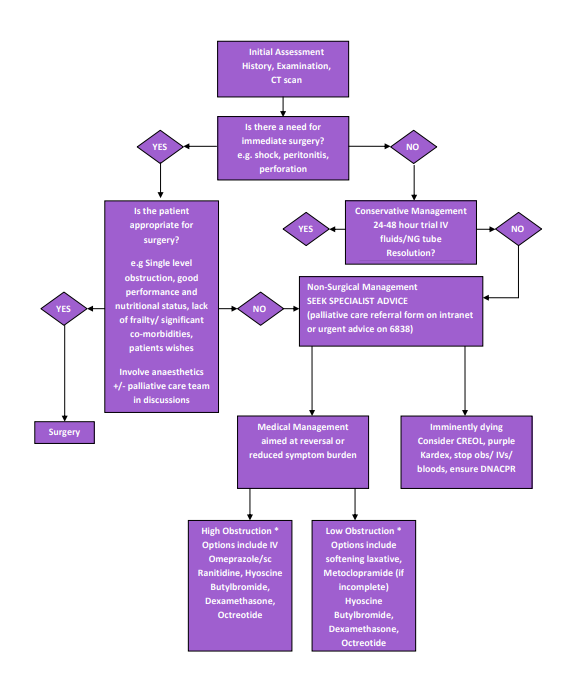
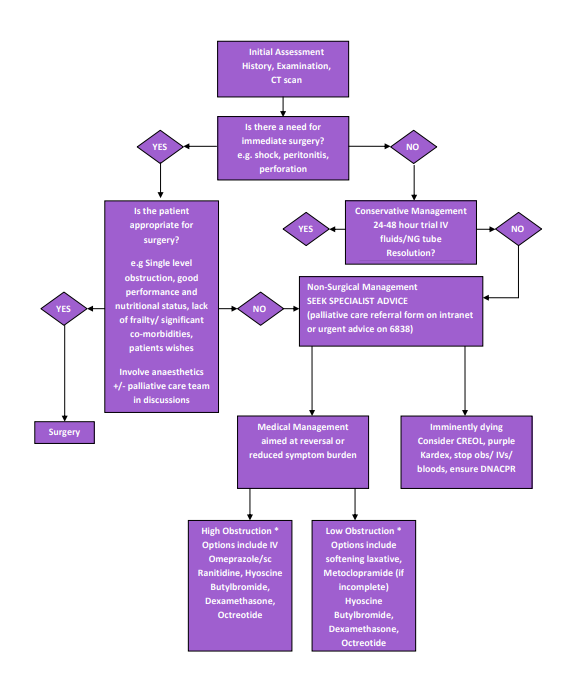
Bowel obstruction – surgical and non-surgical management

Professional guidance and Patient Information Leaflets available on Scottish Palliative Care Guidelines website palliativecareguidelines.scot.nhs.uk
Bowel Obstruction – general guidance
Bowel obstruction may be classified as:
- Permanent/intermittent
- Complete/partial
- Acute/chronic
- Intrinsic/extrinsic
- Mechanical/functional
- High/low
High intestinal obstruction tends to be characterised by vomiting and colicky abdominal pain. Low intestinal obstruction tends to be characterised by abdominal distension and constipation, though vomiting may develop.
Approximately 9 litres of fluids pass through the small bowel per day (oral intake, saliva, GI secretions). High intestinal obstructions tend to produce more fluid and medications such as iv Omeprazole 40mg od, or sc Ranitidine 150-300mg/24hrs can reduce volume of vomits. Laxatives may not be required. Conversely, lower incomplete abdominal obstructions may respond to laxatives such as Docusate or Laxido (caution with the latter as requires the patient to swallow a volume of liquid which they may be unable to tolerate).
Metoclopramide is prokinetic and may help in a subacute obstruction, but should be avoided in complete obstruction, and discontinued if usage leads to colic.
Dexamethasone 6-16mg may be of benefit in high or low intestinal obstruction, whether complete or incomplete. Octreotide should be used under specialist advice only, but may reduce the amount of fluid secreted by a blocked intestine, as well as reducing secretions associated with inflamed tumours.
Remember good oral hygiene for all patients, including ice, artificial saliva, and oral sponges. Palliative fluid/diet may be appropriate in some patients. Intravenous or subcutaneous fluids may be indicated in some patients but sensitive discussion is required.
Review current medications in line with cause of obstruction – for example avoiding constipating medications (such as Amitriptyline, Ondansetron – though the latter may be used for nausea in cases of complete obstruction), use of prokinetic/laxatives if partial obstruction/avoid if complete. Do not combine medications with competing modes of action e.g. anticholinergics such as Cyclizine with Metoclopramide.
Consider route of medications in vomiting patients, or patients who are unlikely to absorb well from the stomach. Transdermal routes can be used for stable pain, syringe drivers for unstable pain. Consider carefully whether IV access is indicated in palliative patients. Similarly, if prognosis is expected to be short, consider carefully whether potentially distressing interventions such as bloods and observations are indicated. In these patients, please consider a purple Kardex and commencement of the Care Record for End of Life (CREOL).