This fact sheet provides information on how to treat patients with Multiple Sclerosis (MS) with different symptoms, situations and circumstances.
Please note this fact sheet is only designed as a brief summary of management.

This fact sheet provides information on how to treat patients with Multiple Sclerosis (MS) with different symptoms, situations and circumstances.
Please note this fact sheet is only designed as a brief summary of management.
MS is an inflammatory disease affecting the central nervous system (i.e. brain and spinal cord) and is the most common non-traumatic disabling condition. The cause remains unknown, but a number of associations are known, including: female sex (3:1); cigarette smoking; genetic influences; previous Epstein Barr infection; low vitamin D levels.
The majority of people (90%) with MS present with a relapsing remitting syndrome (RRMS), while the remainder present with a gradually progressive clinical syndrome (Primary Progressive MS).
Before the era of disease modifying therapies, around 2/3 of people with RRMS would enter the secondary progressive stage from 10 to 15 years after their first symptoms. Presenting with MS for the first time before the age of 15, or after 50, is recognised, but unusual.
We receive many referrals from primary care where MS features high on the differential for both GPs and patients. This advice sheet is to help GPs identify which symptoms are more likely to represent the first presentation of MS.

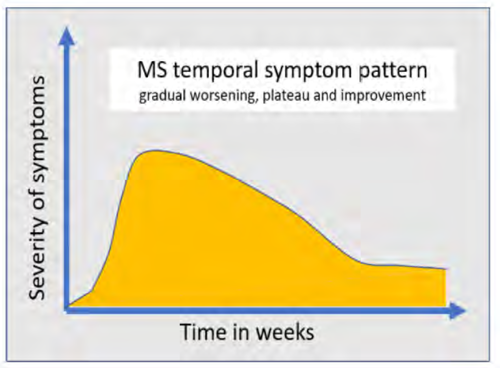
Clinical MS inflammation (relapse) typically presents with a specific focal symptom evolving over hours to days (rarely stroke–like), persisting for days to weeks, then gradually resolving, often completely. Relapses are not characterised by numerous, non-focal symptoms waxing and waning over long periods of time.
Headache, isolated fatigue / tiredness, seizures / blackouts and intermittent sensory symptoms are unlikely to be due to MS. Intermittent sensory symptoms are perhaps the most common symptom referred regarding MS concerns and are usually benign – see the Benign sensory symptoms factsheet. The time course is important - MS symptoms usually worsen over days and persist for weeks while symptoms rarely last minutes or hours at a time.
People with rapidly evolving and disabling neurological symptoms suggestive of MS (see above) should be
referred either via the SCI Gateway, or the on-call neurology team, if the situation is developing very rapidly. Unilateral visual loss may require ophthalmology assessment, initially to exclude primary eye disease.
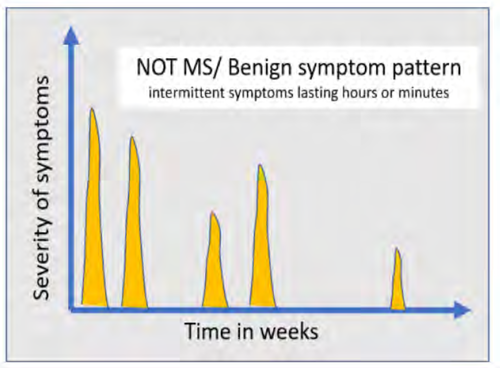
Most people referred with a concern of MS from primary care prove to have an alternative and usually benign diagnosis. The most common are benign sensory symptoms, sometimes nerve entrapment syndromes. Functional neurological disorder can often mimic MS, but is characterised typically by a much broader clinical syndrome than the more monochrome MS presentations listed above (i.e. multiple different symptoms, often with pain and fatigue dominating).
Coles A. Multiple sclerosis. Pract Neurol. 2009 Apr;9(2):118-26. DOI: 10.1136/jnnp.2008.171132