Self-monitoring of blood pressure by pregnant women is going to be rolled out in phases to high-risk women. Home monitoring will be initially targeted to women at high-risk of hypertensive complications or who are ‘shielded’ because of serious underlying medical conditions (Group 1), followed by women identified at increased risk of hypertensive complications (Group 2).
Home blood pressure monitoring should NOT replace any appointment where a woman is receiving clinical review for her underlying medical condition (e.g. for respiratory review of cystic fibrosis or cardiac review of underlying cardiac condition) or where fetal assessment is required as part of the clinical review.
All requests for home BP monitoring in GGC must be discussed and approved by a consultant. The named consultant must have recorded in BadgerNet that they agree to home monitoring and outline the follow-up plan.
Group 1
Women identified as 'high risk' of hypertensive complication including: - Chronic Hypertension
- Current Gestational Hypertension (Pregnancy Induced Hypertension, PIH)
- Current Pre-eclampsia
Women who have been advised to shield because of serious underlying medical conditions: - Cystic Fibrosis
- Solid organ transplant
- Cardiac conditions
|
Group 2
'Increased risk' of developing Pre-eclampsia - Hypertensive disease during a previous pregnancy
- Chronic Kidney Disease
- Autoimmune disease (eg SLE / Antiphospholipid syndrome)
|
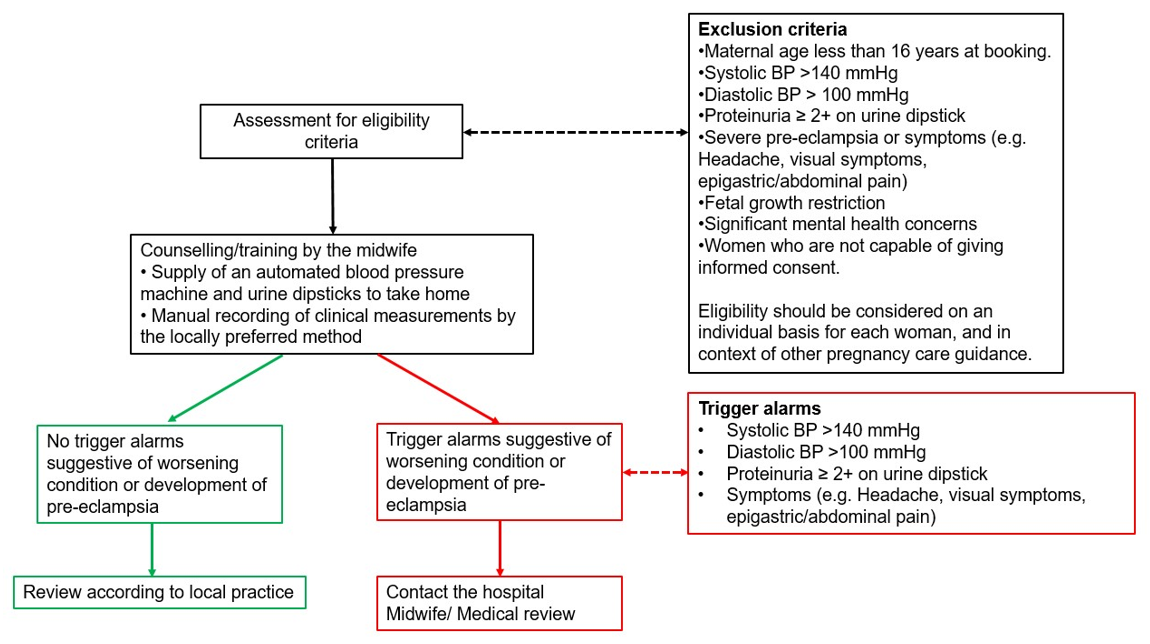
All women being considered for home blood pressure monitoring must fulfil the following clinical inclusion and exclusion criteria:
Inclusion criteria
- Systolic BP range ≤140 mmHg
- Diastolic BP range ≤100 mmHg
- Proteinuria ≤ 1+ on urine dipstick
- Normal full blood count, liver and renal function blood tests as baseline and when new proteinuria present
Exclusion criteria
- Maternal age <16 years at booking.
- Systolic BP >140 mmHg
- Diastolic BP >100 mmHg
- Proteinuria ≥ 2+ on urine dipstick
- Symptoms of headaches, visual symptoms, epigastric pain
- Significant mental health concerns
- Women who are not capable of giving informed consent
- Women who are not able to operate home blood pressure equipment
- Fetal growth restriction
- Women not wishing to take this responsibility
Eligibility should be considered on an individual basis for each woman, and in context of other pregnancy care guidance. Consideration should be given to ensuring that the woman has sufficient digital literacy, data/internet and devices to participate in remote consultations.