Download: Paediatric wound assessment and management chart (pdf)
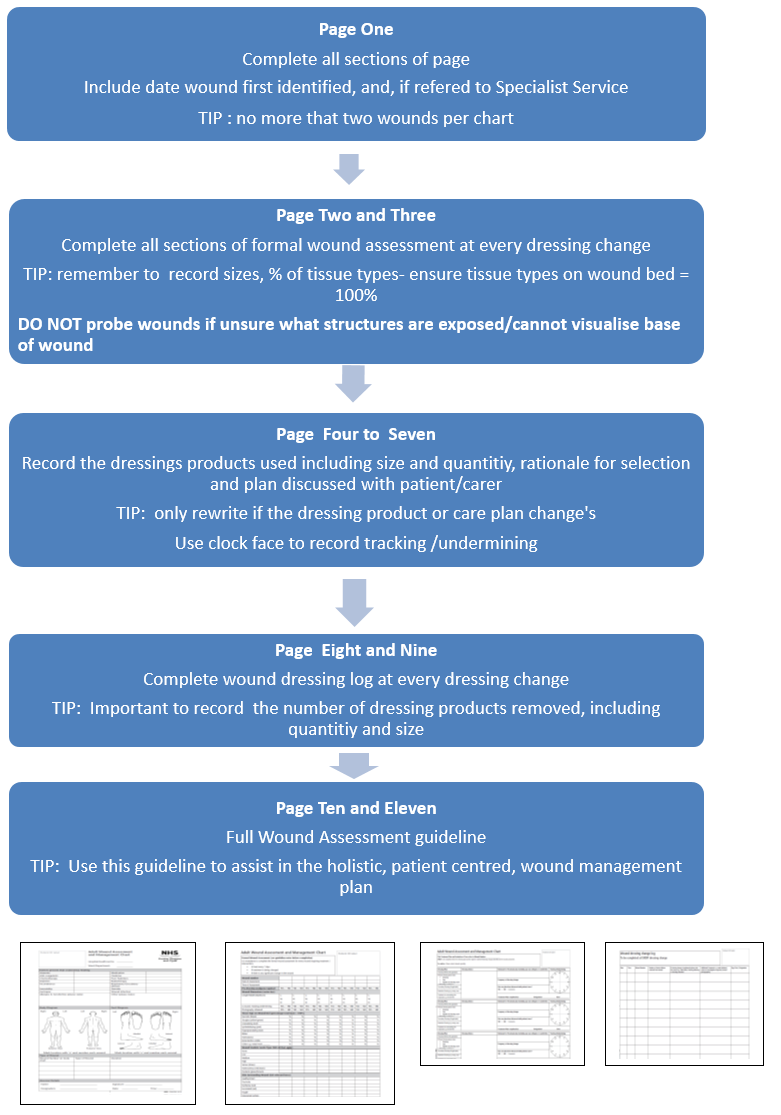
Page 1 - to be completed on initial assessment
- Attach patient label
- Record ward/department and the site (hospital or health centre)
- Identify all factors present which could delay wound healing by ticking the relevant box/boxes
- Use the Other box to add any additional factors that could delay wound healing, i.e. obesity, concordance issues
- Record any known allergies or sensitivities including those to dressing products
- Identify the location of each wound on body or foot diagram. Number each wound (maximum of 2 per wound chart)
- Record wound type and duration of wound to corresponding number - these factors will influence wound management plan
- Record any specialist service details that the child may have been referred to, i.e. Tissue Viability, Physiotherapy, Dietitian, and date when referred
Page 2 & 3 - wound assessment information must be completed for every wound on the initial assessment, every time the wound is reviewed or daily if seen more than once a day.
- Record wound number, date and time of assessment
- Ensure effective pain management/sedation is provided; identify if analgesia/sedation is required prior to/during dressing change. Circle No, Yes, NA (Not Applicable) to describe if analgesia effective, or not required.
- Wound dimensions - measure wound in cm/mm. Use disposable tape measure provided in dressing packs.
- Length is from head to toe
- Width is from right to left
- Depth of wound should be measured
DO NOT PROBE WOUND IF UNSURE WHAT STRUCTURES ARE EXPOSED/YOU CANNOT VISUALISE THE BASE OF THE WOUND.
- Record if tracking or undermining is present to help identify full extend of wound and possibility of sinus/fistula
- Record direction of undermining/ tracking on clock face diagram in treatment plan (page 4-7)
- Record if photographic record is obtained - N.B written consent is required and photographs can only be taken by Medical Illustration/authorised camera users and stored within a secure system as per policy [Staffnet link].
- The type of tissues present will help identify stage of healing and treatment objectives.
- Identify tissue types on wound bed and record percentages of each tissue type to obtain 100%. This will identify if treatment objectives are being achieved.
- Wound Exudate - identify exudate levels and record type of exudates
| Descriptor | Description |
| None | Wound tissues dry |
| Low | Wound tissues wet, moisture evenly distributed in wound <25% of dressing soiled |
| Medium | Wound tissues saturated, drainage may or may not be evenly distributed in wound, 25%-75% of dressing soiled |
| High | Wound tissues bathed in fluid, drainage freely expressed, may or may not be evenly distributed in the wound, >75% of dressing soiled |
| Serous | Clear, light colour, Thin, watery |
| Haemoserous | Light red to pink, Thin, watery |
| Purulent / Pus | Yellow, tan to green, Thick, opaque |
- Record the skin condition around the wound
- Monitor for signs of infection and obtain wound swab if infection suspected
- Treatment objectives - determine treatment objectives to guide dressing choice and plan care
- Record assessors details in line with requirement for record keeping
Pages 4-7 - Treatment plan
ONLY to be completed when the dressing type and/or regime is initiated/altered following changes identified at wound assessment. For advice speak to relevant specialty.
Complete information in dressing choice section as indicated for:
- Method of cleansing if required (refer to wound cleansing guidelines)
- Record if any product is to be applied to surrounding skin e.g. for protection
- Primary dressing including size and number of dressing pieces used
When inserting dressing product into a cavity wound, ensure end of every dressing piece is left above skin surface and size/number of pieces of dressing used is recorded on application/removal to ensure there is no risk of dressing products being retained in the wound.
- Secondary dressing used if applicable
- Any retention dressing required such as bandages
- Rationale for treatment plan - record objective of treatment to allow effectiveness and appropriateness of treatment to be evaluated
- Record frequency for each dressing change
- Comments - Record whether wound care has been discussed with the patient/parents/carers to ensure care is patient centred
- Draw line to indicate direction of Tracking/Undermining on clock face diagram with 12 o'clock referring to head, 3 o'clock to patient's left side, 6 o'clock referring to feet, and 9 o'clock to patient's right side
- Record assessors details
- Use continuation sheet as required
- If there is a change in care plan then discontinue previous care plan by one score through, initial and date
Page 5 - wound dressing change log
- Complete at EVERY dressing change
- Record date and time
- Record number for corresponding wound as noted on the wound assessment chart
- Record the number of dressing pieces removed from the wound, refer to number of pieces applied from previous dressing application (as per treatment plan) to ensure no dressing products are retained within the wound
- Record reason for any unplanned wound dressing changes
- Provide additional comments as required such as when wound photographed, wound swab obtained for culture and sensitivity, investigations requested or feedback from patient
- Sign your record of care, print name and designation
- Use continuation sheet as required