Identifying appropriate oxygen saturations
- Oximeters from different manufacturers may give different saturation readings depending on whether fractional or functional oxygen saturation is being measured.
- Target oxygen saturations are:
- 94-98% in children and adults(3)
- 91-95% (Saturation monitor limits 89-95%) in neonates <1500g or<32 weeks
- >92% (Saturation monitor limits 91-98%) in those discharged from ROP screening and all other babies(4).
- Variable in cyanotic heart disease
- The median baseline oxygen saturation in healthy term infants is 97- 98% in the first year of life(5)
- The median baseline oxygen saturation in children > 1year is 98% with 5th percentile 96-97%.(5)
- Consequences of low oxygen saturation(5) o Pulmonary hypertension. Saturations >94% appear to reduce pulmonary hypertension, whereas saturations <88-90% appear to cause pulmonary hypertension. This does not apply to all children with congenital cardiac defects or idiopathic pulmonary hypertension.
- Adverse effects on behaviour when <88%. Effects of milder hypoxia less clear.
- In infants with chronic neonatal lung disease saturation <90% is associated with increased risk of apparent life threatening events. In same group saturations <92% are associated with poor growth and <90% is associated with poor sleep quality
- Consequences of excess oxygen therapy o Can be toxic in preterm infants causing increased chronic lung disease and retinopathy of prematurity (4). No data in older children.
- Can cause CO2 retention in susceptible patients such as those with chronic neuromuscular disorders, chest wall deformities, cystic fibrosis, morbid obesity and ex premature babies with chronic lung disease, It has also been shown to occur in patients presenting with severe exacerbations of asthma(2),
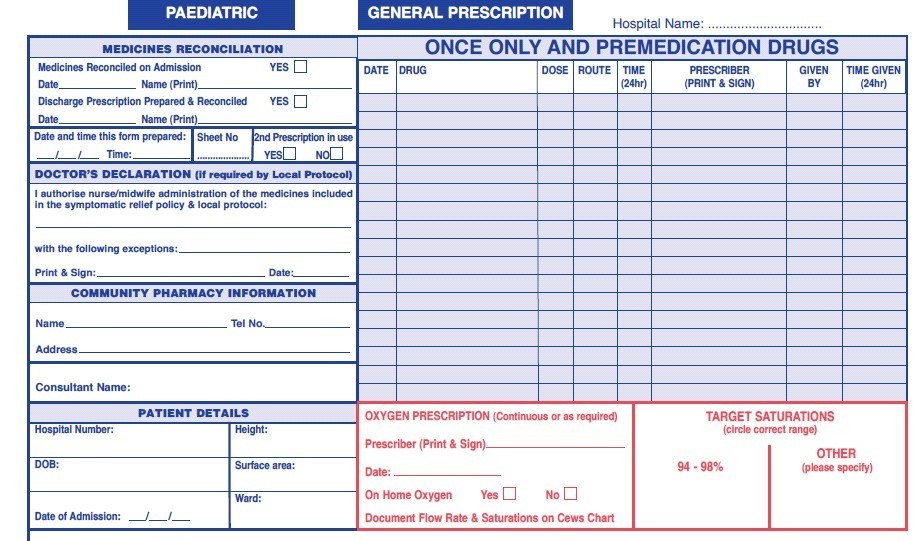
Prescribing oxygen on the drug chart (Appendix a)
An oxygen section on the drug chart has been designed to assist prescription and administration. Oxygen should be prescribed by a doctor in the designated section of the hospital prescription card and the appropriate target saturation should be circled on the chart.
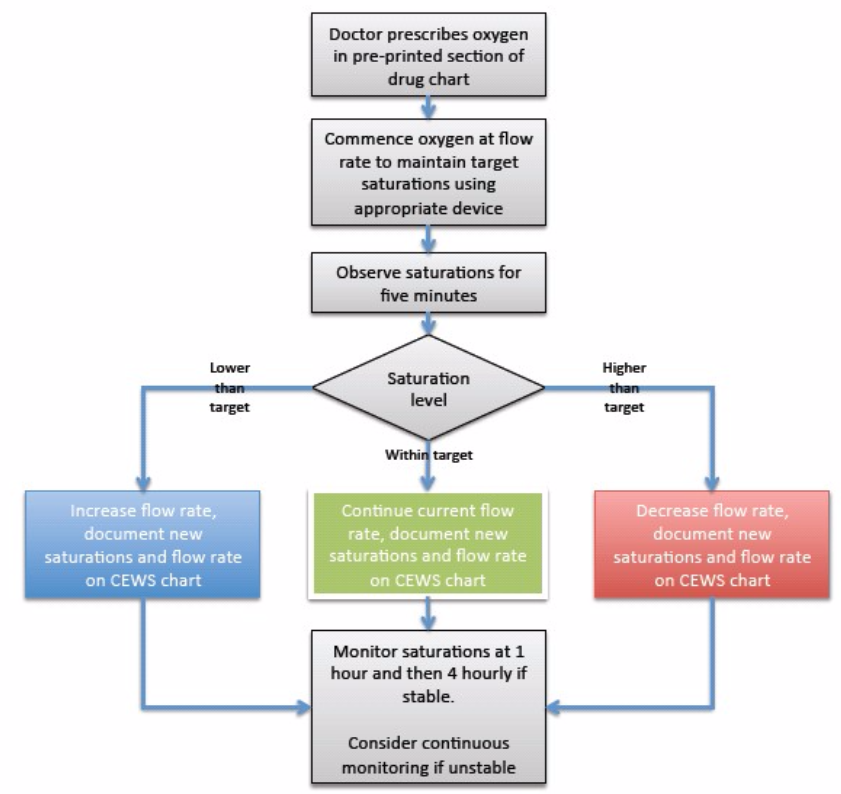
Administering oxygen (Appendix b)
Once the target saturation has been identified and prescribed, guidance regarding the most appropriate delivery system to reach and maintain the prescribed saturation is provided for those administering oxygen.
|
ACTION
|
RATIONALE
|
|
All patients requiring oxygen therapy will have a prescription for oxygen therapy recorded on the patients drug prescription chart. N.B exceptions- see emergency situations
|
Oxygen should be regarded as a drug and should be prescribed. BTS National guidelines (2008). British National Formulary (2008).
|
|
The prescription will incorporate a target saturation that will be identified by the clinician prescribing the oxygen.
|
Certain groups of patients require different target ranges for their oxygen saturation
|
|
Patients should have their oxygen saturation observed immediately after starting oxygen for at least five minutes, after one hour and then four hourly depending on the clinical status of the patient. Oxygen saturations should be recorded on the CEWS chart.
|
To identify if oxygen therapy is maintaining the target saturation or if an increase or decrease in oxygen therapy is required
|
|
The oxygen flow rate should be recorded alongside the oxygen saturation on the bedside observation (CEWS) chart.
|
To provide an accurate record and allow trends in oxygen therapy and saturation levels to be identified.
|
|
Oxygen saturations must always be interpreted alongside the patient’s clinical status incorporating the early warning score (CEWS).
|
To identify early signs of clinical deterioration, e.g. elevated respiratory rate
|
|
If the patient falls outside the target saturation range, the oxygen therapy will be adjusted accordingly.Saturations should then be monitored continuously for at least 5 minutes and recorded on the CEWS chart after any increase or decreasein oxygen dose to ensure that the patient acheives the desired saturation range.
|
To maintain the saturation in the desired range.
|
|
Saturation higher than target specified or >98% for an extended period of time.
|
|
- Step down oxygen therapy as per guidance for delivery
|
The patient will require weaning down from current oxygen delivery system.
|
- Consider discontinuation of oxygen therapy
|
The patients clinical condition may have improved negating the need for
supplementary oxygen
|
|
Saturation lower than target specified
|
|
- Step up oxygen therapy as per protocols. Any sudden fall in oxygen saturation should lead to clinical evaluation.
|
To assess the patients response to oxygen increase and to review the cause of deteriorating oxygen level. Consider need to check capillary blood gas for CO2 level.
|
- Monitor Early Warning Score (CEWS) and respiratory rate for further clinical signs of deterioration
|
Patient safety
|
- Check all elements of oxygen delivery system for faults or errors.
|
In most instances a fall in oxygen saturation is due to deterioration of the patient however equipment faults should be checked for.
|
|
Saturation within target specified
|
|
- Continue with oxygen therapy, and monitor patient to identify appropriate time for stepping down therapy, once clinical condition allows
|
|
- A change in delivery device (without an increase in O2 therapy) does not require review by the medical team.
|
(The change may be made in stable patients due to patient preference or comfort).
|
Oxygen delivery methods
The selection of an appropriate oxygen delivery system must take into account, clinical condition, the patient's size, needs and therapeutic goals (6)
Face Mask
Supplied in children sizes but children do not always tolerate them (7). There are two types of facemasks and selection depends on the condition of the child (8):
- Simple Oxygen Mask (Variable flow masks)
Vents in the mask allow for the dilution of oxygen (9).
Guide to oxygen concentration:
5- 6 lpm = 35-50%
6 -10 lpm = 50-60%
10 - 12 lpm = 60-65%
- High concentration oxygen Masks (non rebreathe masks)
Used for emergency situations (Advanced Life Support Group, 1997) due to a large reservoir that allows oxygen only to be breathed in by the child. This prevents the inhalation of mixed gases. The approximate inspired oxygen received is 99% (10).
- High flow oxygen devices (eg. Vapotherm)
Nasal cannula device capable of giving high flows up to 8L/min in infants and 40L/min in older children and adults without drying secretions as the oxygen is warmed to body temperature and saturated with water vapour. Please see separate guidelines for ward use in bronchiolitis and PICU use.
Humidification
Humidified oxygen should be used when high concentration of oxygen is required for prolonged periods and in those with chronic respiratory illness to prevent drying of the mucosa and secretions (9). Although there is no evidence that nasal cannula oxygen needs to be humidified our current policy in RHSC is to use cold humidification at all flow rates.
Wafting
When conventional delivery methods are not tolerated, wafting of oxygen via a face mask has been shown to deliver concentrations of 30% - 40% with 10 litres oxygen per minute, to an area of 35 x 32cms from top of the mask. Wafting via green oxygen tubing has been assessed as appropriate for short- term use only, i.e., whilst feeding. A standard paediatric oxygen mask placed on the chest can give significant oxygen therapy with minimal distress to the patient (11).
Via nebulisation
Nebulisers should be delivered via oxygen and not air.
Tracheostomy
Oxygen can be delivered via a tracheostomy mask (4-15L/min) or Swedish nose (0.125-4L/min). Consider child’s individual needs.
Nasal Cannula
Can be used for long-term oxygen use, whilst allowing the child to vocalise and eat. The concentration is often not controlled resulting in a low inspiratory oxygen concentration. The use of nasal cannulae can cause dermatitis and mucosal drying (Joint Formulary Committee, 2006). Nasal cannula oxygen does not need to be humidified.
Via a ventilation circuit
Accurate measurement of inspired oxygen is difficult and pulse oximetry must be maintained. Can be delivered at various points throughout the ventilation circuit (12).
Via an Ayres T piece – open ended bag
Used frequently by anaesthetists and gives a reliable impression of the state of the lungs. This technique allows manual application of PEEP (Positive End-Expiratory Pressure). It is completely reliant on an effective oxygen source (Advanced Life Support Group, 2003).
Bag valve mask
Come in three sizes: 250 mls, 500 mls and 1500 mls. The smallest one is ineffective even at birth. Two smallest bags have a pressure-limiting valve set at 4.41 kPa (45 cm H20) to protect the lungs from barotrauma (Damage caused to tissues by a change in pressure inside and outside the body). The reservoir bag enables the delivery of oxygen concentrations up to 98%. Without the reservoir bag it is not possible to supply more than 50% oxygen
(Advanced Life Support Group, 2003)
Monitoring and recording oxygen (See appendix b)
The patient's oxygen saturation and oxygen flow rate should be recorded on the bedside observation chart alongside other physiological variables.
All patients on oxygen therapy should have regular pulse oximetry measurements. The frequency of oximetry measurements will depend on the condition being treated and the stability of the patient.
- All patients should be monitored for the first 5 minutes after starting oxygen or a after a change in flow rate.
- Assuming the patient remains stable, saturations should be checked after one hour and then at least four hourly Critically ill patients should have their oxygen saturations monitored continuously and recorded every few minutes
- Each saturation check should be recorded on the observation chart
- Oxygen therapy should be increased if the saturation is below the desired range and decreased if the saturation is above the desired range (and eventually discontinued as the patient recovers).
- Any change in oxygen requirement should be recorded on the observation chart.
- Any sudden fall in oxygen saturation should lead to clinical evaluation of the patient.
- Patients should be monitored accurately for signs of improvement or deterioration. Nurses should also monitor skin colour for peripheral cyanosis and respiratory rate.
- Oxygen saturations of less than 90%, with or without oxygen, laboured breathing or respiratory rate, or change in CEWS score outwith the expected range for the child should be reported immediately to the medical team.
Emergency situations
In the emergency situation an oxygen prescription is not required. Oxygen should be given to the patient immediately without a formal prescription or drug order but documented later in the patient’s record.
All peri-arrest and critically ill patients should be given 100% oxygen (15 l/m reservoir mask) whilst awaiting immediate medical review. Patients with risk factors for hypercapnia who develop critical illness should have the same initial target saturations as other critically ill patients pending the results of urgent blood gas results after which these patients may need controlled oxygen therapy or supported ventilation if there is severe hypoxaemia and/or hypercapnia with respiratory acidosis.
All patients who have had a respiratory arrest or cardiac arrest should have 100% oxygen provided along with basic/advanced life support.
A subsequent written record must be made of what oxygen therapy has been given to every patient alongside the recording of all other emergency treatment.
Any qualified nurse/ health professional can commence oxygen therapy in an emergency situation.